|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
T
|
ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
|
|
£
|
TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934
|
|
Delaware
|
42-1406317
|
|
|
(State or other jurisdiction of
incorporation or organization)
|
(I.R.S. Employer
Identification Number)
|
|
|
7700 Forsyth Boulevard
|
||
|
St. Louis, Missouri
|
63105
|
|
|
(Address of principal executive offices)
|
(Zip Code)
|
|
Common Stock, $0.001 Par Value
|
New York Stock Exchange
|
|
|
Title of Each Class
|
Name of Each Exchange on Which Registered
|
|
Part I
|
||||
|
Item 1.
|
|
|
2
|
|
|
Item 1A.
|
11
|
|||
|
Item 1B.
|
17
|
|||
|
Item 2.
|
|
|
17
|
|
|
Item 3.
|
|
|
17
|
|
|
Item 4.
|
17
|
|||
|
Part II
|
||||
|
Item 5.
|
|
|
17
|
|
|
Item 6.
|
|
|
19
|
|
|
Item 7.
|
|
|
20
|
|
|
Item 7A.
|
|
|
29
|
|
|
Item 8.
|
|
|
30
|
|
|
Item 9.
|
|
|
50
|
|
|
Item 9A.
|
|
|
50
|
|
|
Item 9B.
|
|
|
52
|
|
|
Part III
|
||||
|
Item 10.
|
|
|
52
|
|
|
Item 11.
|
|
|
52
|
|
|
Item 12.
|
|
|
52
|
|
|
Item 13
|
|
|
52
|
|
|
Item 14.
|
|
|
52
|
|
|
Part IV
|
||||
|
Item 15.
|
|
|
52
|
|
|
|
54
|
|||
|
·
|
our ability to accurately predict and effectively manage health benefits and other operating expenses;
|
|
·
|
competition;
|
|
·
|
changes in healthcare practices;
|
|
·
|
changes in federal or state laws or regulations;
|
|
·
|
inflation;
|
|
·
|
provider contract changes;
|
|
·
|
new technologies;
|
|
·
|
reduction in provider payments by governmental payors;
|
|
·
|
major epidemics;
|
|
·
|
disasters and numerous other factors affecting the delivery and cost of healthcare;
|
|
·
|
the expiration, cancellation or suspension of our Medicaid managed care contracts by state governments;
|
|
·
|
availability of debt and equity financing, on terms that are favorable to us; and
|
|
·
|
general economic and market conditions.
|
|
·
|
Strong Historic Operating Performance.
We have increased revenues as we have grown in existing markets, expanded into new markets and broadened our product offerings. We entered the Wisconsin market in 1984, the Indiana market in 1995, the Texas market in 1999, the Arizona market in 2003, the Ohio market in 2004, the Georgia market in 2006, the South Carolina market in 2007, the Florida and Massachusetts markets in 2009 and the Mississippi market in 2011. We have increased our membership through participation in new programs in existing states. For example, in 2008, we began operations in the Texas Foster Care program and began serving Acute Care members in Yavapai county of Arizona. We have also increased membership by acquiring Medicaid businesses, contracts and other related assets from competitors in existing markets, most recently in Florida and South Carolina in 2010.
Our at-risk membership totaled approximately 1.5 million as of December 31, 2010. For the year ended December 31, 2010, we had revenues of $4.4 billion, representing a 25% Compound Annual Growth Rate, or CAGR, since the year ended December 31, 2005. We generated total cash flow from operations of $168.9 million and net earnings of $90.9 million for the year ended December 31, 2010.
|
|
·
|
Medicaid Expertise.
For more than 25 years, we have developed a specialized Medicaid expertise that has helped us establish and maintain relationships with members, providers and state governments. We have implemented programs developed to achieve savings for state governments and improve medical outcomes for members by reducing inappropriate emergency room use, inpatient days and high cost interventions, as well as by managing care of chronic illnesses. Our experience in working with state regulators helps us implement and deliver programs and services efficiently and affords us opportunities to provide input regarding Medicaid industry practices and policies in the states in which we operate. We work with state agencies on redefining benefits, eligibility requirements and provider fee schedules in order to maximize the number of uninsured individuals covered through Medicaid, CHIP, Foster Care and ABD and expand the types of benefits offered. Our approach is to accomplish this while maintaining adequate levels of provider compensation and protecting our profitability.
|
|
·
|
Diversified Business Lines.
We continue to broaden our service offerings to address areas that we believe have been traditionally underserved by Medicaid managed care organizations. In addition to our Medicaid and Medicaid-related managed care services, our service offerings include behavioral health, health insurance exchanges, individual health insurance, life and health management, long-term care programs, managed vision, telehealth services and pharmacy benefits management. Through the utilization of a multi-business line approach, we are able to improve quality of care, improve outcomes, and diversify our revenues and help control our medical costs.
|
|
·
|
Localized Approach with Centralized Support Infrastructure.
We take a localized approach to managing our subsidiaries, including provider and member services. This approach enables us to facilitate access by our members to high quality, culturally sensitive healthcare services. Our systems and procedures have been designed to address these community-specific challenges through outreach, education, transportation and other member support activities. For example, our community outreach programs work with our members and their communities to promote health and self-improvement through employment and education on how best to access care. We complement this localized approach with a centralized infrastructure of support functions such as finance, information systems and claims processing, which allows us to minimize general and administrative expenses and to integrate and realize synergies from acquisitions. We believe this combined approach allows us to efficiently integrate new business opportunities in both Medicaid and specialty services while maintaining our local accountability and improved access.
|
|
·
|
Specialized and Scalable Systems and Technology.
Through our specialized information systems, we work to strengthen relationships with providers and states which help us grow our membership base. We continue to develop our specialized information systems which allow us to support our core processing functions under a set of integrated databases, designed to be both replicable and scalable. Physicians can use claims, utilization and membership data to manage their practices more efficiently, and they also benefit from our timely payments. State agencies can use data from our information systems to demonstrate that their Medicaid populations receive quality healthcare in an efficient manner. These systems also help identify needs for new healthcare and specialty programs. We have the ability to leverage our platform for one state configuration into new states or for health plan acquisitions. Our utilization data is maintained on one common system for all health plans. Our ability to access data and translate it into meaningful information is essential to operating across a multi-state service area in a cost-effective manner.
|
|
·
|
Increase Penetration of Existing State Markets.
We seek to continue to increase our Medicaid membership in states in which we currently operate through alliances with key providers, outreach efforts, development and implementation of community-specific products and acquisitions. In Texas, we expanded our operations to the Corpus Christi market in 2006, began managing care for ABD recipients in February 2007 and began operations in the Foster Care program in April 2008. In Arizona, we began serving members of a long-term care plan in 2006 and within an acute care plan in 2008. In 2008, we began serving Medicare members within Special Needs Plans in Arizona, Ohio, Texas and Wisconsin. We may also increase membership by acquiring Medicaid businesses, contracts and other related assets from our competitors in our existing markets or by enlisting additional providers. For example, in 2010, we acquired certain Medicaid-related assets in Florida and South Carolina.
|
|
·
|
Diversify Business Lines.
We seek to broaden our business lines into areas that complement our existing business to enable us to grow and diversify our revenue. We are constantly evaluating new opportunities for expansion both domestically and abroad. For instance, in July 2008, we completed the acquisition of Celtic Insurance Company, a national individual health insurance provider. In October 2006, we commenced operations under our managed care program contracts to provide long-term care services in Arizona, and in January 2006, we completed the acquisition of US Script, a pharmacy benefits manager. We employ a disciplined acquisition strategy that is based on defined criteria including internal rate of return, accretion to earnings per share, market leadership and compatibility with our information systems. We engage our executives in the relevant operational units or functional areas to ensure consistency between the diligence and integration process.
|
|
·
|
Address Emerging State Needs.
We work to assist the states in which we operate in addressing the operating challenges they face. We seek to assist the states in balancing premium rates, benefit levels, member eligibility, policies and practices, and provider compensation. For example, in November 2010, we began operating under a new contract with the Texas Department of Insurance to provide affordable health plans for Texas small businesses under the new Healthy Texas initiative, in April 2010, we began offering an individual insurance product for residents of Massachusetts who do not qualify for other state funded insurance programs and in 2008, we began operating under a contract with the Texas Health and Human Services Commission for Comprehensive Health Care for Children in Foster Care, a new statewide program providing managed care services to participants in the Texas Foster Care program. By helping states structure an appropriate level and range of Medicaid, CHIP and specialty services, we seek to ensure that we are able to continue to provide those services on terms that achieve targeted gross margins, provide an acceptable return and grow our business.
|
|
·
|
Develop and Acquire Additional State Markets.
We continue to leverage our experience to identify and develop new markets by seeking both to acquire existing business and to build our own operations. We expect to focus expansion in states where Medicaid recipients are mandated to enroll in managed care organizations, because we believe member enrollment levels are more predictable in these states. In addition, we focus on states where managed care programs can help address states’ financial needs. In 2007, we entered the South Carolina market and we participated in the state’s conversion to at-risk managed care. In February 2009, we began managed care operations in Florida through conversion of members in certain counties from Access Health Solutions to at-risk managed care in Sunshine State Health Plan, through our state contract. In July 2009, we began operating under our contract in Massachusetts to manage healthcare services operating as CeltiCare Health Plan of Massachusetts. In 2011, we began managing care for ABD members in Mississippi. We expect to begin
providing managed care services to older adults and adults with disabilities in Illinois in the first half of 2011.
|
|
·
|
Leverage Established Infrastructure to Enhance Operating Efficiencies
. We intend to continue to invest in infrastructure to further drive efficiencies in operations and to add functionality to improve the service provided to members and other organizations at a low cost. Information technology, or IT, investments complement our overall efficiency goals by increasing the automated processing of transactions and growing the base of decision-making analytical tools. Our centralized functions and common systems enable us to add members and markets quickly and economically.
|
|
·
|
Maintain Operational Discipline.
We monitor our cost trends, operating performance, regulatory relationships and the Medicaid political environment in our existing markets. We seek to operate in markets that allow us to meet our internal metrics including membership growth, plan size, market leadership and operating efficiency. We may divest contracts or health plans in markets where the state’s Medicaid environment, over a long-term basis, does not allow us to meet our targeted performance levels. We use multiple techniques to monitor and reduce our medical costs, including on-site hospital review by staff nurses and involvement of medical management in significant cases. Our executive dashboard is utilized to quickly identify cost drivers and medical trends. Our management team regularly evaluates the financial impact of proposed changes in provider relationships,
contracts, changes in membership and mix of members, potential state rate changes and cost reduction initiatives.
|
|
State
|
Local Health Plan Name
|
|
First Year of Operations Under the Company
|
|
Counties Served at December 31, 2010
|
|
Market Share
(1)
|
At-risk Managed Care Membership at
December 31, 2010
|
|
||
|
Arizona
|
Bridgeway Health Solutions
(2)
|
2008
|
5
|
1.5%
|
22,400
|
||||||
|
Florida
|
Sunshine State Health Plan
|
2009
|
26
|
17.3%
|
194,900
|
||||||
|
Georgia
|
Peach State Health Plan
|
2006
|
90
|
28.6%
|
305,800
|
||||||
|
Indiana
|
Managed Health Services
|
1995
|
92
|
31.8%
|
215,800
|
||||||
|
Massachusetts
|
CeltiCare Health Plan
|
2009
|
14
|
(3)
|
36,200
|
||||||
|
Ohio
|
Buckeye Community Health Plan
|
2004
|
43
|
9.9%
|
160,100
|
||||||
|
South Carolina
|
Absolute Total Care
|
2007
|
42
|
17.2%
|
90,300
|
||||||
|
Texas
|
Superior HealthPlan
|
1999
|
254
|
18.7%
|
433,100
|
||||||
|
Wisconsin
|
Managed Health Services
|
1984
|
38
|
10.5%
|
74,900
|
||||||
|
604
|
1,533,500
|
||||||||||
|
(1)
|
Represents Medicaid and CHIP membership as of December 31, 2010 as a percentage of total eligible Medicaid and CHIP managed care members in each state. ABD programs are excluded.
|
|
(2)
|
Represents the acute care and Medicare businesses under Bridgeway Health Solutions.
|
|
(3)
|
CeltiCare Health Plan manages members under the state Commonwealth Care Bridge program and Commonwealth Care program with market share of 100% and approximately 7.0%, respectively.
|
|
·
|
Significant cost savings and budget predictability compared to state paid reimbursement for services.
We bring bottom-line management experience to our health plans. On the administrative and management side, we bring experience including quality of care improvement methods, utilization management procedures, an efficient claims payment system, and provider performance reporting, as well as managers and staff experienced in using these key elements to improve the quality of and access to care. We receive a contracted premium on a per member basis and are responsible for the medical costs and as a result, provide budget predictability.
|
|
·
|
Data-driven approaches to balance cost and verify eligibility.
Our Medicaid health plans have conducted enrollment processing and activities for state programs since 1984. We seek to ensure effective enrollment procedures that move members into the plan, then educate them and ensure they receive needed services as quickly as possible. Our IT department has created mapping/translation programs for loading membership and linking membership eligibility status to all of Centene’s subsystems.
|
|
·
|
Establishment of realistic and meaningful expectations for quality deliverables.
We have collaborated with state agencies in redefining benefits, eligibility requirements and provider fee schedules with the goal of maximizing the number of individuals covered through Medicaid, CHIP, Foster Care and ABD programs.
|
|
·
|
Managed care expertise in government subsidized programs.
Our expertise in Medicaid has helped us establish and maintain strong relationships with our constituent communities of members, providers and state governments. We provide access to services through local providers and staff that focus on the cultural norms of their individual communities. To that end, systems and procedures have been designed to address community-specific challenges through outreach, education, transportation and other member support activities.
|
|
·
|
Improved medical outcomes.
We have implemented programs developed to achieve savings for state governments and improve medical outcomes for members by reducing inappropriate emergency room use, inpatient days and high cost interventions, as well as by managing care of chronic illness.
|
|
·
|
Timely payment of provider claims.
We are committed to ensuring that our information systems and claims payment systems meet or exceed state requirements. We continuously endeavor to update our systems and processes to improve the timeliness of our provider payments.
|
|
·
|
Provider outreach and programs.
Our health plans have adopted a physician-driven approach where network providers are actively engaged in developing and implementing healthcare delivery policies and strategies. This approach is designed to eliminate unnecessary costs, improve services to members and simplify the administrative burdens placed on providers.
|
|
·
|
Responsible collection and dissemination of utilization data.
We gather utilization data from multiple sources, allowing for an integrated view of our members’ utilization of services. These sources include medical, vision and behavioral health claims and encounter data, pharmacy data, dental vendor claims and authorization data from the authorization and case management system utilized by us to coordinate care.
|
|
·
|
Timely and accurate reporting.
Our information systems have reporting capabilities which have been instrumental in identifying the need for new and/or improved healthcare and specialty programs. For state agencies, our reporting capability is important in demonstrating an auditable program.
|
|
·
|
Fraud and abuse prevention.
We have several systems in place to help identify, detect and investigate potential waste, abuse and fraud including pre and post payment software. We collaborate with state and federal agencies and assist with investigation requests. We use nationally recognized standards to benchmark our processes.
|
|
Ÿ
|
primary and specialty physician care
|
Ÿ
|
transportation assistance
|
|
|
Ÿ
|
inpatient and outpatient hospital care
|
Ÿ
|
vision care
|
|
|
Ÿ
|
emergency and urgent care
|
Ÿ
|
dental care
|
|
|
Ÿ
|
prenatal care
|
Ÿ
|
immunizations
|
|
|
Ÿ
|
laboratory and x-ray services
|
Ÿ
|
prescriptions and limited over-the-counter drugs
|
|
|
Ÿ
|
home health and durable medical equipment
|
Ÿ
|
therapies
|
|
|
Ÿ
|
behavioral health and substance abuse services
|
Ÿ
|
social work services
|
|
|
Ÿ
|
24-hour nurse advice line
|
Ÿ
|
|
Ÿ
|
Start Smart For Your Baby
®
is a prenatal and infant health program designed to increase the percentage of pregnant women receiving early prenatal care, reduce the incidence of low birth weight babies, identify high risk pregnancies, increase participation in the federal Women, Infant and Children program, prevent hospital admissions in the first year of life and increase well-child visits. The program includes risk assessments, education through face-to-face meetings and materials, behavior modification plans, assistance in selecting a provider for the infant and scheduling newborn follow-up visits. These initiatives are supported by a statistically proven reduction in Neonatal Intensive Care Unit (NICU) days as well as increased gestational birth weights. The program includes a Notification of Pregnancy process to identify pregnant women more quickly and enables us to help them gain access to prenatal medical care, give them education on their healthcare needs, assist with social needs and concerns, and coordinate referrals to appropriate specialists and the obstetrics (OB) case management program as needed. The Notification of Pregnancy also identifies women eligible for our high risk OB management program, or 17P Program, which aims to reduce the rate of recurrent preterm delivery and neonatal intensive care admissions through the use of Progesterone. In addition, Start Smart has also co-written a book for the first year of life with the American Academy of Pediatrics. In 2010, Start Smart won the Platinum Award for Consumer Empowerment at the URAC Quality Summit. Start Smart also was awarded the 2010 URAC / GKEN International Health Promotion Award. The “Your Pregnancy Guide” developed by Start Smart was a 2010 Silver Medalist of the National Health Information Award.
|
|
Ÿ
|
Connections Plus
®
is a cell phone program developed for high-risk members who have limited or no access to a safe, reliable telephone. The program puts free, preprogrammed cell phones into the hands of eligible members. This program seeks to eliminate lack of safe, reliable access to a telephone as a barrier to coordinating care, thus reducing avoidable adverse events such as inappropriate emergency room utilization, hospital admissions and premature birth. Members are identified through case management activities or through a referral. Connections Plus is available to high-risk members in all Centene health plans. Originally designed for pregnant women and ABD populations, this program has now been expanded to service members with mental health issues, and specific diseases, including sickle cell. Connections Plus was recognized as a URAC Best Practice 2009 Silver Medalist and a 2008 NCQA Best Practice.
|
|
Ÿ
|
MemberConnections
®
is a community face-to-face outreach and education program designed to create a link between the member and the provider and help identify potential challenges or risk elements to a member’s health, such as nutritional challenges and health education shortcomings. MemberConnections representatives contact new members by phone or mail to discuss managed care, the Medicaid program and our services. Our MemberConnections representatives make home visits, conduct educational programs and represent our health plans at community events such as health fairs.
|
|
Ÿ
|
Thumbs Up Johnnie Health Initiatives for Children
is aimed at educating child members on a variety of health topics. Our health plans are reaching out directly to children with newsletters, contests and other innovative events, such as readings with the author of “The Adventures of Thumbs Up Johnnie” series of books. Thumbs Up Johnnie has developed two programs: preventive obesity and asthma. Obesity rates for children doubled in the past two decades and tripled for adolescents during the same period. Preventive obesity focuses on the childhood obesity epidemic with educational information encouraging proper eating and exercise habits. We have sponsored the creation of a book with author Michelle Bain titled "Thumbs Up Johnnie & the SUPER Centeam 5 - Adventures Through FITROPOLIS!" which is intended to educate children on the importance of living an active and healthy life as well as a kid’s cookbook entitled “SUPER Centeam 5 Cookbook”and a teen book entitled “Off the Chain”. Thumbs Up Johnnie’s focus on asthma has resulted in the creation of the book “Asthma: The Adventures from Puffletown” which educates children about how to manage their asthma. This book received the 2010 National Health Information Award Silver Medal.
|
|
Ÿ
|
Health Passport
is a leading-edge, patient-centric electronic community health record for foster care children in the state of Texas. Passport collects patient demographic data, clinician visit records, dispensed medications, vital sign history, lab results, allergy charts, and immunization data. Providers can directly input additional or updated patient data and documentation into the Passport. All information is accessible anywhere, anytime to all authorized users, including health plan staff, greatly facilitating coordinated care among providers. In 2010, we expanded the Health Passport to our behavioral health program in Arizona.
|
|
Ÿ
|
Fluvention
is an outreach program aimed at educating members on preventing the transmission of the influenza virus by encouraging members to get the seasonal influenza vaccines and take everyday precautions to prevent illness. We use an integrated communications approach including direct mail, phone calls, providing information via health plan websites and posting information in provider offices. The health plans also conduct general community awareness through public service announcements on television and radio. Beginning in 2009, we targeted education efforts related to health hygiene, preventative care and the benefits of obtaining appropriate care of their condition, for groups that are at higher-risk for contracting both the traditional and H1N1 influenza viruses, including pregnant women, children from six months old up to 24-year-old adults, as well as adults with chronic health conditions. Incentives in the form of gift cards were given to members who received both flu vaccines.
|
|
Ÿ
|
EPSDT Case Management
is a preventive care program designed to educate our members on the benefits of Early and Periodic Screening, Diagnosis and Treatment, or EPSDT, services. We have a systematic program of communicating, tracking, outreach, reporting and follow-through that promotes state EPSDT programs.
|
|
Ÿ
|
Life and Health Management Programs
are designed to help members understand their disease and treatment plan and improve their wellness in a cost effective manner. These programs address medical conditions that are common within the Medicaid population such as asthma, diabetes and pregnancy. Our Specialty Services segment manages many of our life and health management programs. Our ABD program uses a proprietary assessment tool that effectively identifies barriers to care, unmet functional needs, available social supports and the existence of behavioral health conditions that impede a member’s ability to maintain a proper health status. Care coordinators develop individual care plans with the member and healthcare providers ensuring the full integration of behavioral, social and acute care services. These care plans, while specific to an ABD member, incorporate “Condition Specific” practices in collaboration with physician partners and community resources.
|
|
Primary Care
Physicians
|
Specialty Care
Physicians
|
Hospitals
|
||||||||||
|
Arizona
|
1,256 | 2,966 | 25 | |||||||||
|
Florida
|
1,785 | 4,290 | 78 | |||||||||
|
Georgia
|
3,056 | 9,831 | 122 | |||||||||
|
Indiana
|
1,036 | 5,443 | 97 | |||||||||
|
Massachusetts
|
1,937 | 6,676 | 35 | |||||||||
|
Ohio
|
2,000 | 8,537 | 122 | |||||||||
|
South Carolina
|
1,519 | 4,501 | 34 | |||||||||
|
Texas
|
8,885 | 21,671 | 400 | |||||||||
|
Wisconsin
|
2,451 | 6,655 | 76 | |||||||||
|
Total
|
23,925 | 70,570 | 989 | |||||||||
|
Ÿ
|
Under our fee-for-service contracts with physicians, particularly specialty care physicians, we pay a negotiated fee for covered services. This model is characterized as having no financial risk for the physician. In addition, this model requires management oversight because our total cost may increase as the units of services increase or as more expensive services replace less expensive services. We have prior authorization procedures in place that are intended to make sure that certain high cost diagnostic and other services are medically appropriate.
|
|
Ÿ
|
Under our capitated contracts, primary care physicians are paid a monthly fee for each of our members assigned to his or her practice for all ambulatory care. In return for this payment, these physicians provide all primary care and preventive services, including primary care office visits and EPSDT services, and are at risk for all costs associated with such services. If these physicians also provide non-capitated services to their assigned members, they may receive payment under fee-for-service arrangements at standard Medicaid rates.
|
|
Ÿ
|
Under risk-sharing arrangements, physicians are paid under a capitated or fee-for-service arrangement. The arrangement, however, contains provisions for additional bonus to the physicians or reimbursement from the physicians based upon cost and quality factors. We often refer to these arrangements as Model 1 contracts.
|
|
Ÿ
|
Customized Utilization Reports
provide certain of our contracted physicians with information that enables them to run their practices more efficiently and focuses them on specific patient needs. For example, quarterly detail reports update physicians on their status within their risk pools. Equivalency reports provide physicians with financial comparisons of capitated versus fee-for-service arrangements.
|
|
Ÿ
|
Case Management Support
helps the physician coordinate specialty care and ancillary services for patients with complex conditions and direct members to appropriate community resources to address both their health and socio-economic needs.
|
|
Ÿ
|
Web-based Claims and Eligibility Resources
have been implemented to provide physicians with on-line access to perform claims and eligibility inquiries.
|
|
Ÿ
|
appropriate leveling of care for neonatal intensive care unit hospital admissions, other inpatient hospital admissions, and observation admissions, in accordance with Interqual criteria;
|
|
Ÿ
|
tightening of our pre-authorization list and more stringent review of durable medical equipment and injectibles;
|
|
Ÿ
|
emergency department, or ED, program designed to collaboratively work with hospitals to steer non-emergency care away from the costly ED setting (through patient education, on-site alternative urgent care settings, etc.);
|
|
Ÿ
|
increase emphasis on case management and clinical rounding where case managers are nurses or social workers who are employed by the health plan to assist selected patients with the coordination of healthcare services in order to meet a patient's specific healthcare needs;
|
|
Ÿ
|
incorporation of disease management, which is a comprehensive, multidisciplinary, collaborative approach to chronic illnesses such as asthma and diabetes; and
|
|
Ÿ
|
Start Smart For Your Baby, a prenatal case management program aimed at helping women with high-risk pregnancies deliver full-term, healthy infants.
|
|
Ÿ
|
Behavioral Health.
Cenpatico Behavioral Health, or Cenpatico, manages behavioral healthcare for members via a contracted network of providers. Cenpatico works with providers to determine the best services to help people overcome mental illness and lead productive lives. Our networks feature a full range of services and levels of care to help people with mental illness reach their recovery and wellness goals. In addition, we operate school-based programs in Arizona that focus on students with special needs and also provide speech and other therapy services. We acquired Cenpatico in 2003.
|
|
Ÿ
|
Individual and State Sponsored Health Insurance Exchanges.
Celtic Insurance Company, or Celtic, is a national healthcare provider licensed in 49 states offering high-quality, affordable health insurance to individual customers and their families. Sold online and through independent insurance agents nationwide, Celtic’s portfolio of major medical plans is designed to meet the diverse needs of the uninsured at all budget and benefit levels. Celtic also offers a standalone guaranteed-issue medical conversion program to self-funded employer groups, stop-loss and fully-insured group carriers, managed care plans, and HMO reinsurers. We acquired Celtic in July 2008. In 2009, CeltiCare of Massachusetts was formed to provide state sponsored health insurance to the uninsured who do not qualify for Medicaid. In 2010, NovaSys Health LLC was acquired to add both TPA and PPO network capabilities.
|
|
Ÿ
|
Life and Health Management.
Nurtur Health, Inc. (Nurtur) specializes in implementing life and health management programs that encourage healthy behaviors, promote healthier workplaces, improve workforce and societal productivity and reduce healthcare costs. Health risk appraisals, biometric screenings, online and telephonic wellness programs, disease management and work-life/employee assistance services are areas of focus. Nurtur Health uses telephonic health and work/life balance coaching, in-home and online interaction and informatics processes to deliver effective clinical outcomes, enhanced patient-provider satisfaction and overall healthcare cost. Nurtur was formed in December 2007 through the combination of three
entities we acquired from July 2005 through November 2007.
|
|
Ÿ
|
Long-term Care and Acute Care.
Bridgeway Health Solutions, or Bridgeway, provides long-term care services to the elderly and people with disabilities that meet income and resources requirements who are at risk of being or are institutionalized. Bridgeway has long-term care members in the Maricopa, Yuma and La Paz counties of Arizona. Bridgeway participates with community groups to address situations that might be barriers to quality care and independent living. Bridgeway commenced long-term care operations in 2006. Bridgeway also provides acute care services to members in the Yavapai county of Arizona. These services include emergency and physician and hospitalization services, limited dental and rehabilitative services and other maternal and child health services. Bridgeway commenced acute care operations in October 2008.
|
|
Ÿ
|
Managed Vision.
OptiCare administers routine and medical surgical eye care benefits via its own contracted national network of eye care providers. OptiCare clients include Medicaid, Medicare, and commercial health plans, as well as employer groups. OptiCare has been providing vision network services for over 25 years and offers a variety of plan designs to meet the individual needs of its clients and members. We acquired the managed vision business of OptiCare Health Systems, Inc. in 2006.
|
|
Ÿ
|
Telehealth Services.
NurseWise and Nurse Response provide a toll-free nurse triage line 24 hours per day, 7 days per week, 52 weeks per year. Our members call one number and reach bilingual customer service representatives and nursing staff who provide health education, triage advice and offer continuous access to health plan functions. Additionally, our representatives verify eligibility, confirm primary care provider assignments and provide benefit and network referral coordination for members and providers after business hours. Our staff can arrange for urgent pharmacy refills, transportation and qualified behavioral health professionals for crisis stabilization assessments. Call volume is based on membership levels and seasonal variation. NurseWise commenced operations in 1998 and Nurse Response was acquired in 2006.
|
|
Ÿ
|
Pharmacy Benefits Management.
US Script offers progressive pharmacy benefits management services that are specifically designed to improve quality of care while containing costs. This is achieved through a lowest net cost strategy that helps optimize clients' pharmacy benefit. Services include claims processing, pharmacy network management, benefit design consultation, drug utilization review, formulary and rebate management, specialty and mail order pharmacy services, patient and physician intervention
.
We acquired US Script in 2006.
|
|
Ÿ
|
Care Management Software.
Casenet is a software provider of innovative care management solutions that automate the clinical, administrative and technical components of care management programs. We maintain an equity investment in Casenet and are currently implementing this new software platform which is available for sale to third parties. We acquired a controlling interest in Casenet in 2010 and present it as a consolidated subsidiary of the Company.
|
|
Ÿ
|
written standards of conduct;
|
|
Ÿ
|
designation of a corporate compliance officer and compliance committee;
|
|
Ÿ
|
effective training and education;
|
|
Ÿ
|
effective lines for reporting and communication;
|
|
Ÿ
|
enforcement of standards through disciplinary guidelines and actions;
|
|
Ÿ
|
internal monitoring and auditing; and
|
|
Ÿ
|
prompt response to detected offenses and development of corrective action plans.
|
|
Ÿ
|
Medicaid Managed Care Organizations
focus on providing healthcare services to Medicaid recipients. These organizations consist of national and regional organizations, as well as smaller organizations that operate in one city or state and are owned by providers, primarily hospitals.
|
|
Ÿ
|
National and Regional Commercial Managed Care Organizations
have Medicaid members in addition to members in private commercial plans. Some of these organizations offer a range of specialty services including pharmacy benefits management, behavioral health management, health management, and nurse triage call support centers.
|
|
Ÿ
|
Primary Care Case Management Programs
are programs established by the states through contracts with primary care providers. Under these programs, physicians provide primary care services to Medicaid recipients, as well as limited medical management oversight.
|
|
Ÿ
|
premium taxes or similar assessments;
|
|
Ÿ
|
stringent prompt-pay laws;
|
|
Ÿ
|
disclosure requirements regarding provider fee schedules and coding procedures; and
|
|
Ÿ
|
programs to monitor and supervise the activities and financial solvency of provider groups.
|
|
Ÿ
|
eligibility, enrollment and disenrollment processes;
|
Ÿ
|
health education and wellness and prevention programs;
|
|
Ÿ
|
covered services;
|
Ÿ
|
timeliness of claims payment;
|
|
Ÿ
|
eligible providers;
|
Ÿ
|
financial standards;
|
|
Ÿ
|
subcontractors;
|
Ÿ
|
safeguarding of member information;
|
|
Ÿ
|
record-keeping and record retention;
|
Ÿ
|
fraud and abuse detection and reporting;
|
|
Ÿ
|
periodic financial and informational reporting;
|
Ÿ
|
grievance procedures; and
|
|
Ÿ
|
quality assurance;
|
Ÿ
|
organization and administrative systems.
|
|
Ÿ
|
accreditation;
|
|
State Contract
|
|
Expiration Date
|
|
Renewal or Extension by the State
|
|
|
Arizona – Acute Care
|
September 30, 2011
|
May be extended for up to two additional one-year terms.
|
|||
|
Arizona – Behavioral Health
|
June 30, 2013
|
Renewable for two additional one-year terms.
|
|||
|
Arizona – Long-term Care
|
September 30, 2011
|
Renewable through the state’s reprocurement process.
|
|||
|
Arizona – Special Needs Plan (Medicare)
|
December 31, 2011
|
Renewable annually for successive 12-month periods.
|
|||
|
Florida – Medicaid & ABD
|
August 31, 2012
|
Renewable through the state’s recertification process.
|
|||
|
Florida – Long-term Care
|
August 31, 2011
|
Renewable through the state’s recertification process.
|
|||
|
Georgia – Medicaid & CHIP
|
June 30, 2011
|
Renewable for three additional one-year terms.
|
|||
|
Indiana – Medicaid & CHIP
|
December 31, 2014
|
Renewable for two additional one-year terms.
|
|||
|
Kansas – Behavioral Health
|
June 30, 2011
|
May be extended for up to one additional one-year term.
|
|||
|
Massachusetts – Commonwealth Care
|
June 30, 2011
|
Renewable through the state’s recertification process.
|
|||
|
Massachusetts – Commonwealth Care Bridge
|
June 30, 2011
|
May be extended for up to three additional one-year terms.
|
|||
|
Mississippi – ABD
|
December 31, 2013
|
Renewable through the state’s recertification process.
|
|||
|
Ohio – Medicaid, CHIP & ABD
|
June 30, 2011
|
Renewable annually for successive 12-month periods.
|
|||
|
Ohio – Special Needs Plan (Medicare)
|
December 31, 2011
|
Renewable annually for successive 12-month periods.
|
|||
|
South Carolina – Medicaid & ABD
|
March 31, 2012
|
May be extended for up to one additional year and subsequently renewable through the state’s recertification process.
|
|||
|
Texas – Medicaid, CHIP & ABD
|
August 31, 2013
|
Renewable through the state’s reprocurement process.
1
|
|||
|
Texas – CHIP Rural Service Area
|
August 31, 2013
|
May be extended for up to five additional years.
|
|||
|
Texas – Foster Care
|
August 31, 2012
|
May be extended for up to three and a half additional years.
|
|||
|
Texas – Special Needs Plan (Medicare)
|
December 31, 2011
|
Renewable annually for successive 12-month periods.
|
|||
|
Wisconsin – Medicaid, CHIP & ABD
|
December 31, 2011
|
Renewable through the state’s recertification process.
|
|||
|
Wisconsin – Network Health Plan Subcontract
|
December 31, 2011
|
Renews automatically for successive five-year terms.
|
|||
|
Wisconsin – Special Needs Plan (Medicare)
|
December 31, 2011
|
Renewable annually for successive 12-month periods.
|
|
Ÿ
|
limit certain uses and disclosures of private health information, and require patient authorizations for such uses and disclosures of private health information;
|
|
Ÿ
|
guarantee patients the right to access their health information and to know who else has accessed it;
|
|
Ÿ
|
limit most disclosure of health information to the minimum needed for the intended purpose;
|
|
Ÿ
|
establish procedures to ensure the protection of private health information;
|
|
Ÿ
|
authorize access to records by researchers and others;
|
|
Ÿ
|
establish requirements for breach notification; and
|
|
Ÿ
|
impose criminal and civil sanctions for improper uses or disclosures of health information.
|
|
Ÿ
|
the state law is necessary to prevent fraud and abuse associated with the provision of and payment for healthcare;
|
|
Ÿ
|
the state law is necessary to ensure appropriate state regulation of insurance and health plans;
|
|
Ÿ
|
the state law is necessary for state reporting on healthcare delivery or costs; or
|
|
Ÿ
|
the state law addresses controlled substances.
|
|
Name
|
|
Age
|
|
Position
|
|
Michael F. Neidorff
|
|
68
|
|
Chairman and Chief Executive Officer
|
|
Karen A. Bedell
|
51
|
Senior Vice President, New Business Integration & Development
|
||
|
Mark W. Eggert
|
49
|
Executive Vice President, Health Plan Business Unit
|
||
|
Carol E. Goldman
|
|
53
|
|
Executive Vice President and Chief Administrative Officer
|
|
Jason M. Harrold
|
41
|
Senior Vice President, Specialty Business Unit
|
||
|
Jesse N. Hunter
|
35
|
Executive Vice President, Corporate Development
|
||
|
Donald G. Imholz
|
58
|
Executive Vice President and Chief Information Officer
|
||
|
Edmund E. Kroll
|
51
|
Senior Vice President, Finance and Investor Relations
|
||
|
Mary V. Mason
|
42
|
Senior Vice President and Chief Medical Officer
|
||
|
William N. Scheffel
|
|
57
|
|
Executive Vice President, Chief Financial Officer and Treasurer
|
|
Jeffrey A. Schwaneke
|
35
|
Vice President, Corporate Controller and Chief Accounting Officer
|
||
|
Keith H. Williamson
|
58
|
Senior Vice President, Secretary and General Counsel
|
|
2010 Stock Price
|
2009 Stock Price
|
|||||||||||||||
|
High
|
Low
|
High
|
Low
|
|||||||||||||
|
First Quarter
|
$ | 25.03 | $ | 17.60 | $ | 22.50 | $ | 15.00 | ||||||||
|
Second Quarter
|
25.95 | 20.51 | 21.00 | 17.29 | ||||||||||||
|
Third Quarter
|
23.65 | 20.00 | 20.48 | 16.89 | ||||||||||||
|
Fourth Quarter
|
26.43 | 21.19 | 22.02 | 17.25 | ||||||||||||
|
Issuer Purchases of Equity Securities
Fourth Quarter 2010
|
|||||||||||
|
Period
|
Total Number of
Shares
Purchased
|
Average Price
Per Share
|
Total Number
of Shares
Purchased as
Publicly
Announced
Plans
or Programs
|
Maximum
Number of Shares
that
May Yet Be
Purchased Under
the Plans or
Programs
|
|||||||
|
October 1 – October 31, 2010
|
949
|
$
|
23.19
|
—
|
1,667,724
|
||||||
|
November 1 – November 30, 2010
|
3,946
|
22.66
|
—
|
1,667,724
|
|||||||
|
December 1 – December 31, 2010
|
99,470
|
24.11
|
—
|
1,667,724
|
|||||||
|
TOTAL
|
|
104,365
|
1
|
$
|
24.04
|
|
—
|
1,667,724
|
|||
|
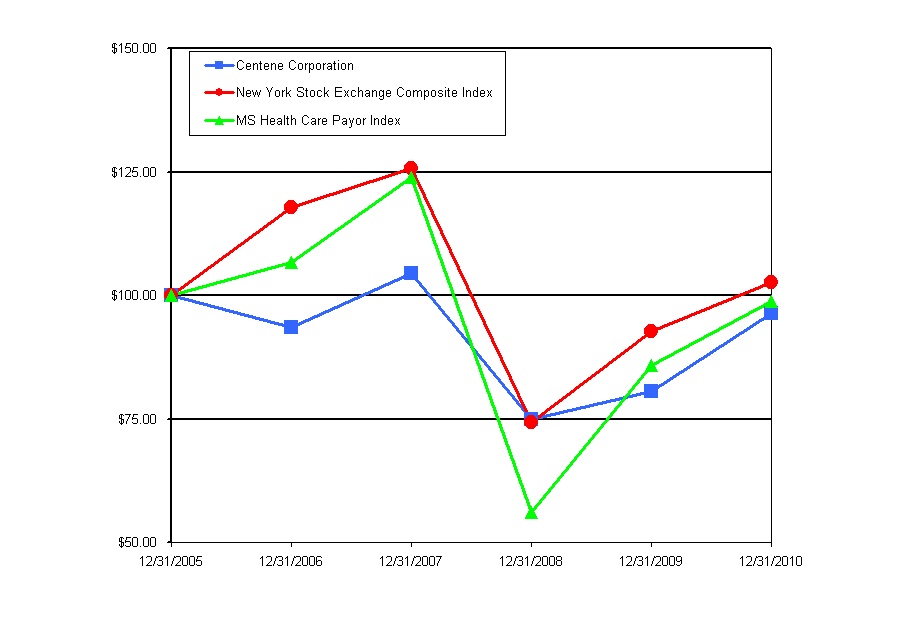
12/31/2005
|
12/31/2006
|
12/31/2007
|
12/31/2008
|
12/31/2009
|
12/31/2010
|
|||||||||||||||||||
|
Centene Corporation
|
$ | 100.00 | $ | 93.46 | $ | 104.37 | $ | 74.97 | $ | 80.52 | $ | 96.39 | ||||||||||||
|
New York Stock Exchange Composite Index
|
$ | 100.00 | $ | 117.86 | $ | 125.62 | $ | 74.25 | $ | 92.66 | $ | 102.71 | ||||||||||||
|
MS Health Care Payor Index
|
$ | 100.00 | $ | 106.65 | $ | 123.92 | $ | 56.00 | $ | 85.91 | $ | 98.96 | ||||||||||||
|
|
Year Ended December 31,
|
|||||||||||||||||||
|
|
2010
|
2009
|
2008
|
2007
|
2006
1
|
|||||||||||||||
|
(In thousands, except share data)
|
||||||||||||||||||||
|
|
||||||||||||||||||||
|
Revenues:
|
|
|||||||||||||||||||
|
Premium
|
|
$
|
4,192,172
|
$
|
3,786,525
|
$
|
3,199,360
|
$
|
2,611,953
|
$
|
1,707,439
|
|||||||||
|
Service
|
|
91,661
|
91,758
|
74,953
|
80,508
|
79,159
|
||||||||||||||
|
Premium and service revenues
|
4,283,833
|
3,878,283
|
3,274,313
|
2,692,461
|
1,786,598
|
|||||||||||||||
|
Premium tax
|
164,490
|
224,581
|
90,202
|
76,567
|
35,848
|
|||||||||||||||
|
Total revenues
|
|
4,448,323
|
4,102,864
|
3,364,515
|
2,769,028
|
1,822,446
|
||||||||||||||
|
Expenses:
|
|
|||||||||||||||||||
|
Medical costs
|
|
3,514,394
|
3,163,523
|
2,640,335
|
2,190,898
|
1,436,371
|
||||||||||||||
|
Cost of services
|
|
63,919
|
60,789
|
56,920
|
61,348
|
60,287
|
||||||||||||||
|
General and administrative expenses
|
|
547,823
|
514,529
|
444,733
|
384,970
|
267,712
|
||||||||||||||
|
Premium tax expense
|
165,118
|
225,888
|
90,966
|
76,567
|
35,848
|
|||||||||||||||
|
Total operating expenses
|
|
4,291,254
|
3,964,729
|
3,232,954
|
2,713,783
|
1,800,218
|
||||||||||||||
|
Earnings from operations
|
|
157,069
|
138,135
|
131,561
|
55,245
|
22,228
|
||||||||||||||
|
Other income (expense):
|
|
|||||||||||||||||||
|
Investment and other income
|
|
15,205
|
15,691
|
21,728
|
24,452
|
15,511
|
||||||||||||||
|
Interest expense
|
|
(17,992
|
)
|
(16,318
|
)
|
(16,673
|
)
|
(15,626
|
)
|
(10,574
|
)
|
|||||||||
|
Earnings from continuing operations, before income tax expense
|
|
154,282
|
137,508
|
136,616
|
64,071
|
27,165
|
||||||||||||||
|
Income tax expense
|
|
59,900
|
48,841
|
52,435
|
23,031
|
9,565
|
||||||||||||||
|
Earnings from continuing operations, net of income tax expense
|
94,382
|
88,667
|
84,181
|
41,040
|
17,600
|
|||||||||||||||
|
Discontinued operations, net of income tax expense (benefit) of $4,388, $(1,204), $(281), $(31,563), and $12,412, respectively
|
3,889
|
(2,422
|
)
|
(684
|
)
|
32,362
|
(61,229
|
)
|
||||||||||||
|
Net earnings (loss)
|
98,271
|
86,245
|
83,497
|
73,402
|
(43,629
|
)
|
||||||||||||||
|
Noncontrolling interest
|
3,435
|
2,574
|
—
|
—
|
—
|
|||||||||||||||
|
Net earnings (loss) attributable to Centene Corporation
|
|
$
|
94,836
|
$
|
83,671
|
$
|
83,497
|
$
|
73,402
|
$
|
(43,629
|
)
|
||||||||
|
Amounts attributable to Centene Corporation common shareholders:
|
||||||||||||||||||||
|
Earnings from continuing operations, net of income tax expense
|
$
|
90,947
|
$
|
86,093
|
$
|
84,181
|
$
|
41,040
|
$
|
17,600
|
||||||||||
|
Discontinued operations, net of income tax expense (benefit)
|
3,889
|
(2,422
|
)
|
(684
|
)
|
32,362
|
(61,229
|
)
|
||||||||||||
|
Net earnings (loss)
|
$
|
94,836
|
$
|
83,671
|
$
|
83,497
|
$
|
73,402
|
$
|
(43,629
|
)
|
|||||||||
|
Net earnings (loss) per common share attributable to Centene Corporation:
|
|
|||||||||||||||||||
|
Basic:
|
||||||||||||||||||||
|
Continuing operations
|
|
$
|
1.87
|
$
|
2.00
|
$
|
1.95
|
$
|
0.95
|
$
|
0.41
|
|||||||||
|
Discontinued operations
|
|
0.08
|
(0.06
|
)
|
(0.02
|
)
|
0.74
|
(1.42
|
)
|
|||||||||||
|
Basic earnings (loss) per common share
|
|
$
|
1.95
|
$
|
1.94
|
$
|
1.93
|
$
|
1.69
|
$
|
(1.01
|
)
|
||||||||
|
Diluted:
|
|
|||||||||||||||||||
|
Continuing operations
|
|
$
|
1.80
|
$
|
1.94
|
$
|
1.90
|
$
|
0.92
|
$
|
0.39
|
|||||||||
|
Discontinued operations
|
|
0.08
|
(0.05
|
)
|
(0.02
|
)
|
0.72
|
(1.37
|
)
|
|||||||||||
|
Diluted earnings (loss) per common share
|
|
$
|
1.88
|
$
|
1.89
|
$
|
1.88
|
$
|
1.64
|
$
|
(0.98
|
)
|
||||||||
|
Weighted average number of common shares outstanding:
|
|
|||||||||||||||||||
|
Basic
|
|
48,754,947
|
43,034,791
|
43,275,187
|
43,539,950
|
43,160,860
|
||||||||||||||
|
Diluted
|
|
50,447,888
|
44,316,467
|
44,398,955
|
44,823,082
|
44,613,622
|
||||||||||||||
|
|
December 31,
|
|||||||||||||||||||
|
|
2010
|
2009
|
2008
|
2007
|
2006
|
|||||||||||||||
|
|
(In thousands)
|
|||||||||||||||||||
|
Consolidated Balance Sheet Data:
|
|
|||||||||||||||||||
|
Cash and cash equivalents
|
|
$
|
433,914
|
$
|
400,951
|
$
|
370,999
|
$
|
267,305
|
$
|
237,514
|
|||||||||
|
Investments and restricted deposits
|
639,983
|
585,183
|
451,058
|
369,545
|
174,431
|
|||||||||||||||
|
Total assets
|
|
1,943,882
|
1,702,364
|
1,451,152
|
1,121,824
|
894,980
|
||||||||||||||
|
Medical claims liability
|
456,765
|
470,932
|
384,360
|
323,741
|
241,073
|
|||||||||||||||
|
Long-term debt
|
|
327,824
|
307,085
|
264,637
|
206,406
|
174,646
|
||||||||||||||
|
Total stockholders’ equity
|
|
797,055
|
619,427
|
501,272
|
415,047
|
326,423
|
||||||||||||||
|
Ÿ
|
Year-end at-risk managed care membership of 1,533,500, an increase of 75,300 members, or 5.2% year over year.
|
|
Ÿ
|
Premium and service revenues from continuing operations of $4.3 billion, representing 10.5% growth year over year.
|
|
Ÿ
|
Health Benefits Ratio from continuing operations of 83.8%, compared to 83.5% in 2009.
|
|
Ÿ
|
General and Administrative expense ratio from continuing operations of 12.8%, compared to 13.3% in 2009.
|
|
Ÿ
|
Diluted net earnings per share from continuing operations of $1.80.
|
|
Ÿ
|
Total operating cash flows of $168.9 million, or 1.7 times net earnings.
|
|
Ÿ
|
Florida.
In February 2009, we began converting non-risk managed care membership from Access Health Solutions LLC, or Access, to our subsidiary, Sunshine State Health Plan on an at-risk basis. During 2010, we completed the conversion of approximately 26,000 members from Access. Additionally, in December 2010, we completed the acquisition of Citrus Health Care, Inc., a Medicaid and long-term care health plan.
|
|
Ÿ
|
South Carolina.
In March 2009, we completed the acquisition of Amerigroup Community Care of South Carolina, Inc. and in June 2010, we completed the acquisition of Carolina Crescent Health Plan. We served 90,300 at-risk members in South Carolina as of December 31, 2010.
|
|
Ÿ
|
Massachusetts.
In July 2009, we began managing healthcare services for members under the state’s Commonwealth Care program and in October 2009 under the Commonwealth Care Bridge program. In April 2010, we began offering an individual insurance product, under the names of Commonwealth Choice and CeltiCare Direct, for residents of the Boston area who do not qualify for other state funded insurance programs. At December 31, 2010, we served 36,200 members operating as CeltiCare Health Plan of Massachusetts.
|
|
Ÿ
|
Arizona.
In December 2010, we began operating under an expanded contract from the Arizona Department of Health Services to manage behavioral healthcare services for an additional four counties including Santa Cruz, Greenlee, Graham and Cochise.
|
|
Ÿ
|
Celtic Insurance Company, Inc.
In July 2010, we closed on the acquisition of certain assets and liabilities of NovaSys Health, LLC, a third party administrator in Arkansas that complements our existing Celtic business. In November 2010, we began operating under a new contract with the Texas Department of Insurance to provide affordable health insurance plans for Texas small businesses under the new Healthy Texas initiative.
|
|
Ÿ
|
In September 2010, our new subsidiary, IlliniCare Health Plan, was selected as one of two vendors to provide managed care services to older adults and adults with disabilities under the Integrated Care Program in six counties of Illinois. We expect operations to commence in the first half of 2011.
|
|
Ÿ
|
In January 2011, we began operating under a new contract in Mississippi to provide managed care services to Medicaid recipients through the Mississippi Coordinated Access Network (MississippiCan) program.
|
|
Ÿ
|
In January 2011, we began operating under a new statewide managed care contract serving Healthy Indiana Plan members.
|
|
Ÿ
|
In February 2011, we began operating under an additional STAR+PLUS ABD contract in Texas in the Dallas service area.
|
|
December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Arizona
|
22,400 | 20,700 | 17,000 | |||||||||
|
Florida
|
194,900 | 102,600 | — | |||||||||
|
Georgia
|
305,800 | 309,700 | 288,300 | |||||||||
|
Indiana
|
215,800 | 208,100 | 175,300 | |||||||||
|
Massachusetts
|
36,200 | 27,800 | — | |||||||||
|
Ohio
|
160,100 | 150,800 | 133,400 | |||||||||
|
South Carolina
|
90,300 | 48,600 | 31,300 | |||||||||
|
Texas
|
433,100 | 455,100 | 428,000 | |||||||||
|
Wisconsin
|
74,900 | 134,800 | 124,800 | |||||||||
|
Total at-risk membership
|
1,533,500 | 1,458,200 | 1,198,100 | |||||||||
|
Non-risk membership
|
4,200 | 63,700 | 3,700 | |||||||||
|
Total
|
1,537,700 | 1,521,900 | 1,201,800 | |||||||||
|
December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Medicaid
|
1,177,100 | 1,081,400 | 877,400 | |||||||||
|
CHIP & Foster Care
|
210,500 | 263,600 | 257,300 | |||||||||
|
ABD & Medicare
|
104,600 | 82,800 | 61,300 | |||||||||
|
Hybrid Programs
|
36,200 | 27,800 | — | |||||||||
|
Long-term Care
|
5,100 | 2,600 | 2,100 | |||||||||
|
Total at-risk membership
|
1,533,500 | 1,458,200 | 1,198,100 | |||||||||
|
Non-risk membership
|
4,200 | 63,700 | 3,700 | |||||||||
|
Total
|
1,537,700 | 1,521,900 | 1,201,800 | |||||||||
|
December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Cenpatico Behavioral Health:
|
||||||||||||
|
Kansas
|
39,200 | 41,400 | 41,100 | |||||||||
|
Arizona
|
174,600 | 120,100 | 105,000 | |||||||||
|
Ÿ
|
acquisitions in Florida and South Carolina;
|
|
Ÿ
|
continued conversion of non-risk membership from Access to at-risk under Sunshine State Health Plan in Florida; and
|
|
Ÿ
|
decreased membership in Texas and Wisconsin as discussed above.
|
|
Ÿ
|
strong organic growth as a result of general economic conditions;
|
|
Ÿ
|
acquisitions in Florida and South Carolina;
|
|
Ÿ
|
the conversion of non-risk membership from Access to at-risk under Sunshine State Health Plan in Florida; and
|
|
Ÿ
|
expansion into Massachusetts under the state Commonwealth Care Bridge and Commonwealth Care programs.
|
|
2010
|
2009
|
2008
|
% Change 2009 - 2010
|
% Change 2008 - 2009
|
||||||||||||||||
|
Premium
|
$ | 4,192.2 | $ | 3,786.5 | $ | 3,199.3 | 10.7 | % | 18.4 | % | ||||||||||
|
Service
|
91.6 | 91.8 | 75.0 | (0.1 | ) % | 22.4 | % | |||||||||||||
|
Premium and service revenues
|
4,283.8 | 3,878.3 | 3,274.3 | 10.5 | % | 18.4 | % | |||||||||||||
|
Premium tax
|
164.5 | 224.6 | 90.2 | (26.8 | ) % | 149.0 | % | |||||||||||||
|
Total revenues
|
4,448.3 | 4,102.9 | 3,364.5 | 8.4 | % | 21.9 | % | |||||||||||||
|
Medical costs
|
3,514.4 | 3,163.5 | 2,640.3 | 11.1 | % | 19.8 | % | |||||||||||||
|
Cost of services
|
63.9 | 60.8 | 56.9 | 5.1 | % | 6.8 | % | |||||||||||||
|
General and administrative expenses
|
547.8 | 514.6 | 444.7 | 6.5 | % | 15.7 | % | |||||||||||||
|
Premium tax expense
|
165.1 | 225.9 | 91.0 | (26.9 | ) % | 148.3 | % | |||||||||||||
|
Earnings from operations
|
157.1 | 138.1 | 131.6 | 13.7 | % | 5.0 | % | |||||||||||||
|
Investment and other income, net
|
(2.8 | ) | (0.6 | ) | 5.0 | 344.5 | % | (112.4 | )% | |||||||||||
|
Earnings from continuing operations, before income tax expense
|
154.3 | 137.5 | 136.6 | 12.2 | % | 0.7 | % | |||||||||||||
|
Income tax expense
|
59.9 | 48.8 | 52.4 | 22.6 | % | (6.9 | )% | |||||||||||||
|
Earnings from continuing operations, net of income tax expense
|
94.4 | 88.7 | 84.2 | 6.4 | % | 5.3 | % | |||||||||||||
|
Discontinued operations, net of income tax expense (benefit) of $4.4, $(0.3) and $(31.6) respectively
|
3.9 | (2.4 | ) | (0.7 | ) | (260.6 | )% | 254.1 | % | |||||||||||
|
Net earnings
|
98.3 | 86.3 | 83.5 | 13.9 | % | 3.3 | % | |||||||||||||
|
Noncontrolling interest
|
3.5 | 2.6 | — | 33.4 | % | — | ||||||||||||||
|
Net earnings attributable to Centene Corporation
|
$ | 94.8 | $ | 83.7 | $ | 83.5 | 13.3 | % | 0.2 | % | ||||||||||
|
Amounts attributable to Centene Corporation common shareholders:
|
||||||||||||||||||||
|
Earnings from continuing operations, net of income tax expense
|
$ | 90.9 | $ | 86.1 | $ | 84.2 | 5.6 | % | 2.3 | % | ||||||||||
|
Discontinued operations, net of income tax expense (benefit)
|
3.9 | (2.4 | ) | (0.7 | ) | (260.6 | )% | 254.1 | % | |||||||||||
|
Net earnings
|
$ | 94.8 | $ | 83.7 | $ | 83.5 | 13.3 | % | 0.2 | % | ||||||||||
|
Diluted earnings (loss) per common share attributable to Centene Corporation:
|
||||||||||||||||||||
|
Continuing operations
|
$ | 1.80 | $ | 1.94 | $ | 1.90 | (7.2 | ) % | 2.1 | % | ||||||||||
|
Discontinued operations
|
0.08 | (0.05 | ) | (0.02 | ) | (260.0 | )% | (150.0 | )% | |||||||||||
|
Total diluted earnings per common share
|
$ | 1.88 | $ | 1.89 | $ | 1.88 | (0.5 | )% | 0.5 | % | ||||||||||
|
Year Ended December 31,
|
||||||||
|
2010
|
2009
|
|||||||
|
Medicaid and CHIP
|
83.6 | % | 84.6 | % | ||||
|
ABD and Medicare
|
85.0 | 81.1 | ||||||
|
Specialty Services
|
83.4 | 80.2 | ||||||
|
Total
|
83.8 | 83.5 | ||||||
|
Year Ended December 31,
|
||||||||
|
2010
|
2009
|
|||||||
|
Investment income
|
$ | 14.9 | $ | 15.6 | ||||
|
Net gain on sale of investments
|
2.5 | 0.1 | ||||||
|
Impairment of investment
|
(5.5 | ) | — | |||||
|
Gain on Reserve Primary Fund distributions
|
3.3 | — | ||||||
|
Interest expense
|
(18.0 | ) | (16.3 | ) | ||||
|
Investment and other income, net
|
$ | (2.8 | ) | $ | (0.6 | ) | ||
|
2010
|
2009
|
% Change
2009-2010
|
||||||||||
|
Premium and Service Revenues
|
||||||||||||
|
Medicaid Managed Care
|
$ | 3,740.5 | $ | 3,464.8 | 8.0 | % | ||||||
|
Specialty Services
|
1,112.1 | 1,049.5 | 6.0 | % | ||||||||
|
Eliminations
|
(568.8 | ) | (636.0 | ) | (10.6 | ) % | ||||||
|
Consolidated Total
|
$ | 4,283.8 | $ | 3,878.3 | 10.5 | % | ||||||
|
Earnings from Operations
|
||||||||||||
|
Medicaid Managed Care
|
$ | 117.1 | $ | 99.3 | 17.9 | % | ||||||
|
Specialty Services
|
40.0 | 38.8 | 2.9 | % | ||||||||
|
Consolidated Total
|
$ | 157.1 | $ | 138.1 | 13.7 | % | ||||||
|
Year Ended December 31,
|
||||||||
|
2009
|
2008
|
|||||||
|
Medicaid and CHIP
|
84.6 | % | 80.6 | % | ||||
|
ABD and Medicare
|
81.1 | 91.1 | ||||||
|
Specialty Services
|
80.2 | 83.8 | ||||||
|
Total
|
83.5 | 82.5 | ||||||
|
Ÿ
|
recording the Georgia premium rate increase for the period from July 1, 2007 to December 31, 2007 during the first quarter of 2008 had the effect of decreasing the HBR in 2008 by 0.6%;
|
|
Ÿ
|
a March 1, 2009 rate decrease for our CHIP/Perinate product in Texas which brought the HBR more in line with our normal range;
|
|
Ÿ
|
higher HBR in our Florida market; and
|
|
Ÿ
|
additional costs related to the flu.
|
|
The following table summarizes the components of investment and other income, net ($ in millions):
|
|
Year Ended December 31,
|
||||||||
|
2009
|
2008
|
|||||||
|
Investment income
|
$ | 15.7 | $ | 19.8 | ||||
|
Earnings from equity method investee
|
— | 6.4 | ||||||
|
Loss on Reserve Primary Fund
|
— | (4.5 | ) | |||||
|
Interest expense
|
(16.3 | ) | (16.7 | ) | ||||
|
Investment and other income, net
|
$ | (0.6 | ) | $ | 5.0 | |||
|
2009
|
2008
|
% Change
2008-2009
|
||||||||||
|
Premium and Service Revenues
|
||||||||||||
|
Medicaid Managed Care
|
$ | 3,464.8 | $ | 2,992.3 | 15.8 | % | ||||||
|
Specialty Services
|
1,049.5 | 816.5 | 28.5 | % | ||||||||
|
Eliminations
|
(636.0 | ) | (534.5 | ) | 19.0 | % | ||||||
|
Consolidated Total
|
$ | 3,878.3 | $ | 3,274.3 | 18.4 | % | ||||||
|
Earnings from Operations
|
||||||||||||
|
Medicaid Managed Care
|
$ | 99.3 | $ | 108.4 | (8.4 | ) % | ||||||
|
Specialty Services
|
38.8 | 23.2 | 67.4 | % | ||||||||
|
Consolidated Total
|
$ | 138.1 | $ | 131.6 | 5.0 | % | ||||||
|
Year Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Net cash provided by operating activities
|
$
|
168.9
|
$
|
248.2
|
$
|
222.0
|
||||||
|
Net cash used in investing activities
|
(210.6
|
)
|
(270.1
|
)
|
(153.9
|
)
|
||||||
|
Net cash provided by financing activities
|
72.1
|
46.6
|
42.4
|
|||||||||
|
Net increase in cash and cash equivalents
|
$
|
30.4
|
$
|
24.7
|
$
|
110.5
|
||||||
|
Year Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Premium and related receivables
|
$
|
(23.4
|
)
|
$
|
2.4
|
$
|
(1.5)
|
|||||
|
Unearned revenue
|
25.7
|
78.3
|
(36.5)
|
|||||||||
|
Net increase (decrease) in operating cash flow
|
$
|
2.3
|
$
|
80.7
|
$
|
(38.0)
|
||||||
|
2010
|
2009
|
|||||||
|
Cash, cash equivalents and short-term investments
|
$ | 455.2 | $ | 440.5 | ||||
|
Long-term investments
|
595.9 | 525.5 | ||||||
|
Restricted deposits
|
22.8 | 20.1 | ||||||
|
Total cash, investments and restricted deposits
|
$ | 1,073.9 | $ | 986.1 | ||||
|
Regulated cash, investments and restricted deposits
|
$ | 1,043.0 | $ | 949.9 | ||||
|
Unregulated cash and investments
|
30.9 | 36.2 | ||||||
|
Consolidated Total
|
$ | 1,073.9 | $ | 986.1 | ||||
|
Regulated cash and investments from discontinued operations
1
|
$ | 4.2 | $ | 24.9 | ||||
|
________________________
1
Upon payment of remaining UHP medical claims liabilities and other liabilities, substantially all of the remaining regulated cash of UHP will be transferred to our unregulated cash.
|
||||||||
|
Payments Due by Period
|
||||||||||||||||||||
|
Total
|
Less Than
1 Year
|
1-3
Years
|
3-5
Years
|
More Than
5 Years
|
||||||||||||||||
|
Medical claims liability
|
$ | 456,765 | $ | 456,765 | $ | — | $ | — | $ | — | ||||||||||
|
Debt
|
330,641 | 2,817 | 6,496 | 189,492 | 131,836 | |||||||||||||||
|
Operating lease obligations
|
67,797 | 18,444 | 25,119 | 14,370 | 9,864 | |||||||||||||||
|
Purchase obligations
|
42,887 | 21,066 | 16,440 | 4,981 | 400 | |||||||||||||||
|
Interest on long-term debt
1
|
44,406 | 12,688 | 25,375 | 6,343 | — | |||||||||||||||
|
Reserve for uncertain tax positions
|
1,668 | 515 | 1,153 | — | — | |||||||||||||||
|
Other long-term liabilities
2
|
52,055 | — | 18,084 | 7,288 | 26,683 | |||||||||||||||
|
Total
|
$ | 996,219 | $ | 513,295 | $ | 92,667 | $ | 222,474 | $ | 168,783 | ||||||||||
|
________________________________
1
Interest on $175,000 Senior Notes.
2
Includes $8,326 separate account liabilities from third party
reinsurance that will not be settled in cash.
|
||||||||||||||||||||
|
Completion Factors (1):
|
|
Cost Trend Factors (2):
|
|||||||||
|
(Decrease)
Increase
in Factors
|
|
Increase
(Decrease) in
Medical Claims
Liabilities
|
(Decrease)
Increase
in Factors
|
|
Increase
(Decrease) in
Medical Claims
Liabilities
|
||||||
|
|
(in thousands)
|
|
(in thousands)
|
||||||||
|
(2.0
|
)%
|
$
|
63,000
|
(2.0
|
)%
|
$
|
(15,900
|
)
|
|||
|
(1.5
|
)
|
|
47,000
|
(1.5
|
)
|
(11,900
|
)
|
||||
|
(1.0
|
)
|
|
31,100
|
(1.0
|
)
|
(7,900
|
)
|
||||
|
(0.5
|
)
|
|
15,600
|
(0.5
|
)
|
(4,000
|
)
|
||||
|
0.5
|
|
(15,400
|
)
|
0.5
|
4,000
|
||||||
|
1.0
|
|
(30,500
|
)
|
1.0
|
8,100
|
||||||
|
1.5
|
|
(45,500
|
)
|
1.5
|
12,100
|
||||||
|
2.0
|
|
(60,500
|
)
|
2.0
|
16,200
|
||||||
|
(1)
|
Reflects estimated potential changes in medical claims liability caused by changes in completion factors.
|
|
(2)
|
Reflects estimated potential changes in medical claims liability caused by changes in cost trend factors for the most recent periods.
|
|
|
Year Ended December 31,
|
|||||||||||
|
|
2010
|
2009
|
2008
|
|||||||||
|
Balance, January 1
|
|
$
|
470,932
|
$
|
384,360
|
$
|
323,741
|
|||||
|
Acquisitions
|
|
—
|
—
|
15,398
|
||||||||
|
Incurred related to:
|
|
|||||||||||
|
Current year
|
|
3,582,463
|
3,216,533
|
2,659,036
|
||||||||
|
Prior years
|
|
(68,069
|
)
|
(53,010
|
)
|
(18,701
|
)
|
|||||
|
Total incurred
|
|
3,514,394
|
3,163,523
|
2,640,335
|
||||||||
|
Paid related to:
|
|
|||||||||||
|
Current year
|
|
3,133,527
|
2,752,983
|
2,292,150
|
||||||||
|
Prior years
|
|
395,034
|
323,968
|
302,964
|
||||||||
|
Total paid
|
|
3,528,561
|
3,076,951
|
2,595,114
|
||||||||
|
Balance, December 31
|
|
$
|
456,765
|
$
|
470,932
|
$
|
384,360
|
|||||
|
|
||||||||||||
|
Claims inventory, December 31
|
|
434,900
|
423,400
|
269,300
|
||||||||
|
Days in claims payable
1
|
|
45.6
|
50.1
|
49.9
|
||||||||
|
________________________
1
Days in claims payable is a calculation of medical claims liability at the end of the period divided by average expense per calendar day for the fourth quarter of each year.
|
||||||||||||
|
Ÿ
|
Appropriate leveling of care for neonatal intensive care unit hospital admissions, other inpatient hospital admissions, and observation admissions, in accordance with Interqual criteria.
|
|
Ÿ
|
Tightening of our pre-authorization list and more stringent review of durable medical equipment and injectibles.
|
|
Ÿ
|
Emergency department, or ED, program designed to collaboratively work with hospitals to steer non-emergency care away from the costly ED setting (through patient education, on-site alternative urgent care settings, etc.)
|
|
Ÿ
|
Increase emphasis on case management and clinical rounding where case managers are nurses or social workers who are employed by the health plan to assist selected patients with the coordination of healthcare services in order to meet a patient's specific healthcare needs.
|
|
Ÿ
|
Incorporation of disease management which is a comprehensive, multidisciplinary, collaborative approach to chronic illnesses such as asthma.
|
|
Intangible Asset
|
Amortization Period
|
|
|
Purchased contract rights
|
5 – 15 years
|
|
|
Provider contracts
|
5 – 10 years
|
|
|
Customer relationships
|
5 – 15 years
|
|
|
Trade names
|
7 – 20 years
|
|
December 31,
2010
|
December 31,
2009
|
|||||||
|
ASSETS
|
||||||||
|
Current assets:
|
||||||||
|
Cash and cash equivalents of continuing operations
|
$ | 433,914 | $ | 400,951 | ||||
|
Cash and cash equivalents of discontinued operations
|
252 | 2,801 | ||||||
|
Total cash and cash equivalents
|
434,166 | 403,752 | ||||||
|
Premium and related receivables, net of allowance for uncollectible accounts of $17 and $1,338, respectively
|
136,243 | 103,456 | ||||||
|
Short-term investments, at fair value (amortized cost $21,141 and $39,230, respectively)
|
21,346 | 39,554 | ||||||
|
Other current assets
|
64,154 | 64,866 | ||||||
|
Current assets of discontinued operations other than cash
|
912 | 4,506 | ||||||
|
Total current assets
|
656,821 | 616,134 | ||||||
|
Long-term investments, at fair value (amortized cost $585,862 and $514,256, respectively)
|
595,879 | 525,497 | ||||||
|
Restricted deposits, at fair value (amortized cost $22,755 and $20,048, respectively)
|
22,758 | 20,132 | ||||||
|
Property, software and equipment, net of accumulated depreciation of $138,629 and $103,883, respectively
|
326,341 | 230,421 | ||||||
|
Goodwill
|
278,051 | 224,587 | ||||||
|
Intangible assets, net
|
29,109 | 22,479 | ||||||
|
Other long-term assets
|
30,057 | 36,829 | ||||||
|
Long-term assets of discontinued operations
|
4,866 | 26,285 | ||||||
|
Total assets
|
$ | 1,943,882 | $ | 1,702,364 | ||||
|
LIABILITIES AND STOCKHOLDERS’ EQUITY
|
||||||||
|
Current liabilities:
|
||||||||
|
Medical claims liability
|
$ | 456,765 | $ | 470,932 | ||||
|
Accounts payable and accrued expenses
|
185,218 | 132,001 | ||||||
|
Unearned revenue
|
117,344 | 91,644 | ||||||
|
Current portion of long-term debt
|
2,817 | 646 | ||||||
|
Current liabilities of discontinued operations
|
3,102 | 20,685 | ||||||
|
Total current liabilities
|
765,246 | 715,908 | ||||||
|
Long-term debt
|
327,824 | 307,085 | ||||||
|
Other long-term liabilities
|
53,378 | 59,561 | ||||||
|
Long-term liabilities of discontinued operations
|
379 | 383 | ||||||
|
Total liabilities
|
1,146,827 | 1,082,937 | ||||||
|
Commitments and contingencies
|
||||||||
|
Stockholders’ equity:
|
||||||||
|
Common stock, $.001 par value; authorized 100,000,000 shares; 52,172,037 issued and 49,616,824 outstanding at December 31, 2010, and 45,593,383 issued and 43,179,373 outstanding at December 31, 2009
|
52 | 46 | ||||||
|
Additional paid-in capital
|
384,206 | 281,806 | ||||||
|
Accumulated other comprehensive income:
|
||||||||
|
Unrealized gain on investments, net of tax
|
6,424 | 7,348 | ||||||
|
Retained earnings
|
453,743 | 358,907 | ||||||
|
Treasury stock, at cost (2,555,213 and 2,414,010 shares, respectively)
|
(50,486 | ) | (47,262 | ) | ||||
|
Total Centene stockholders’ equity
|
793,939 | 600,845 | ||||||
|
Noncontrolling interest
|
3,116 | 18,582 | ||||||
|
Total stockholders’ equity
|
797,055 | 619,427 | ||||||
|
Total liabilities and stockholders’ equity
|
$ | 1,943,882 | $ | 1,702,364 | ||||
|
Year Ended December 31,
|
||||||||||||
|
|
2010
|
2009
|
2008
|
|||||||||
|
Revenues:
|
|
|||||||||||
|
Premium
|
|
$
|
4,192,172
|
$
|
3,786,525
|
$
|
3,199,360
|
|||||
|
Service
|
|
91,661
|
91,758
|
74,953
|
||||||||
|
Premium and service revenues
|
4,283,833
|
3,878,283
|
3,274,313
|
|||||||||
|
Premium tax
|
164,490
|
224,581
|
90,202
|
|||||||||
|
Total revenues
|
|
4,448,323
|
4,102,864
|
3,364,515
|
||||||||
|
Expenses:
|
|
|||||||||||
|
Medical costs
|
|
3,514,394
|
3,163,523
|
2,640,335
|
||||||||
|
Cost of services
|
|
63,919
|
60,789
|
56,920
|
||||||||
|
General and administrative expenses
|
|
547,823
|
514,529
|
444,733
|
||||||||
|
Premium tax expense
|
165,118
|
225,888
|
90,966
|
|||||||||
|
Total operating expenses
|
|
4,291,254
|
3,964,729
|
3,232,954
|
||||||||
|
Earnings from operations
|
|
157,069
|
138,135
|
131,561
|
||||||||
|
Other income (expense):
|
|
|||||||||||
|
Investment and other income
|
|
15,205
|
15,691
|
21,728
|
||||||||
|
Interest expense
|
|
(17,992
|
)
|
(16,318
|
)
|
(16,673
|
)
|
|||||
|
Earnings from continuing operations, before income tax expense
|
|
154,282
|
137,508
|
136,616
|
||||||||
|
Income tax expense
|
|
59,900
|
48,841
|
52,435
|
||||||||
|
Earnings from continuing operations, net of income tax expense
|
94,382
|
88,667
|
84,181
|
|||||||||
|
Discontinued operations, net of income tax expense (benefit) of $4,388, $(1,204) and $(281), respectively
|
3,889
|
(2,422
|
)
|
(684
|
)
|
|||||||
|
Net earnings
|
98,271
|
86,245
|
83,497
|
|||||||||
|
Noncontrolling interest
|
3,435
|
2,574
|
—
|
|||||||||
|
Net earnings attributable to Centene Corporation
|
|
$
|
94,836
|
$
|
83,671
|
$
|
83,497
|
|||||
|
Amounts attributable to Centene Corporation common shareholders:
|
||||||||||||
|
Earnings from continuing operations, net of income tax expense
|
$
|
90,947
|
$
|
86,093
|
$
|
84,181
|
||||||
|
Discontinued operations, net of income tax expense (benefit)
|
3,889
|
(2,422
|
)
|
(684
|
)
|
|||||||
|
Net earnings
|
$
|
94,836
|
$
|
83,671
|
$
|
83,497
|
||||||
|
Net earnings (loss) per common share attributable to Centene Corporation:
|
|
|||||||||||
|
Basic:
|
||||||||||||
|
Continuing operations
|
|
$
|
1.87
|
$
|
2.00
|
$
|
1.95
|
|||||
|
Discontinued operations
|
|
0.08
|
(0.06
|
)
|
(0.02
|
)
|
||||||
|
Basic earnings per common share
|
|
$
|
1.95
|
$
|
1.94
|
$
|
1.93
|
|||||
|
Diluted:
|
|
|||||||||||
|
Continuing operations
|
|
$
|
1.80
|
$
|
1.94
|
$
|
1.90
|
|||||
|
Discontinued operations
|
|
0.08
|
(0.05
|
)
|
(0.02
|
)
|
||||||
|
Diluted earnings per common share
|
|
$
|
1.88
|
$
|
1.89
|
$
|
1.88
|
|||||
|
Weighted average number of common shares outstanding:
|
|
|||||||||||
|
Basic
|
|
48,754,947
|
43,034,791
|
43,275,187
|
||||||||
|
Diluted
|
|
50,447,888
|
44,316,467
|
44,398,955
|
||||||||
|
Centene Stockholders’ Equity
|
||||||||||||||||||||||||||
|
Common Stock
|
Treasury Stock
|
|||||||||||||||||||||||||
|
$.001 Par
Value
Shares
|
Amt
|
Additional
Paid-in
Capital
|
Accumulated
Other
Comprehensive
Income
|
Retained
Earnings
|
$.001 Par
Value
Shares
|
Amt
|
Non
controlling
Interest
|
Total
|
||||||||||||||||||
|
Balance,
December 31, 2007
|
44,532,394
|
$
|
45
|
$
|
239,178
|
$
|
1,571
|
$
|
191,739
|
864,557
|
$
|
(17,486)
|
$
|
—
|
$
|
415,047
|
||||||||||
|
Comprehensive Earnings:
|
||||||||||||||||||||||||||
|
Net earnings
|
—
|
—
|
—
|
—
|
83,497
|
—
|
—
|
—
|
83,497
|
|||||||||||||||||
|
Change in unrealized investment gains, net of $882 tax
|
—
|
—
|
—
|
1,581
|
—
|
—
|
—
|
—
|
1,581
|
|||||||||||||||||
|
Total comprehensive earnings
|
—
|
—
|
—
|
—
|
—
|
—
|
—
|
—
|
85,078
|
|||||||||||||||||
|
Common stock issued for employee benefit plans
|
538,785
|
—
|
6,229
|
—
|
—
|
—
|
—
|
—
|
6,229
|
|||||||||||||||||
|
Common stock repurchases
|
—
|
—
|
—
|
—
|
—
|
1,218,858
|
(23,510)
|
—
|
(23,510
|
)
|
||||||||||||||||
|
Stock compensation expense
|
—
|
—
|
15,328
|
—
|
—
|
—
|
—
|
—
|
15,328
|
|||||||||||||||||
|
Excess tax benefits from stock compensation
|
3,100
|
3,100
|
||||||||||||||||||||||||
|
Balance,
December 31, 2008
|
45,071,179
|
$
|
45
|
$
|
263,835
|
$
|
3,152
|
$
|
275,236
|
2,083,415
|
$
|
(40,996)
|
$
|
—
|
$
|
501,272
|
||||||||||
|
Consolidation of Access Health Solutions LLC
|
—
|
—
|
—
|
—
|
—
|
—
|
—
|
29,144
|
29,144
|
|||||||||||||||||
|
Consolidation of Centene Center LLC
|
—
|
—
|
—
|
—
|
—
|
—
|
—
|
17,400
|
17,400
|
|||||||||||||||||
|
Comprehensive Earnings:
|
||||||||||||||||||||||||||
|
Net earnings
|
—
|
—
|
—
|
—
|
83,671
|
—
|
—
|
2,574
|
86,245
|
|||||||||||||||||
|
Change in unrealized investment gains, net of $2,663 tax
|
—
|
—
|
—
|
4,196
|
—
|
—
|
—
|
—
|
4,196
|
|||||||||||||||||
|
Total comprehensive earnings
|
90,441
|
|||||||||||||||||||||||||
|
Common stock issued for employee benefit plans
|
522,204
|
1
|
3,284
|
—
|
—
|
—
|
—
|
3,285
|
||||||||||||||||||
|
Common stock repurchases
|
—
|
—
|
—
|
—
|
—
|
332,595
|
(6,304)
|
—
|
(6,304
|
)
|
||||||||||||||||
|
Treasury stock issued for compensation
|
—
|
—
|
—
|
—
|
(2,000)
|
38
|
38
|
|||||||||||||||||||
|
Stock compensation expense
|
—
|
—
|
14,634
|
—
|
—
|
—
|
—
|
—
|
14,634
|
|||||||||||||||||
|
Excess tax benefits from stock compensation
|
—
|
—
|
53
|
—
|
—
|
—
|
—
|
—
|
53
|
|||||||||||||||||
|
Conversion fee
1
|
—
|
—
|
—
|
—
|
—
|
—
|
—
|
(27,366)
|
(27,366
|
)
|
||||||||||||||||
|
Distributions to noncontrolling interest
|
—
|
—
|
—
|
—
|
—
|
—
|
—
|
(3,170)
|
(3,170
|
)
|
||||||||||||||||
|
Balance,
December 31, 2009
|
45,593,383
|
$
|
46
|
$
|
281,806
|
$
|
7,348
|
$
|
358,907
|
2,414,010
|
$
|
(47,262)
|
$
|
18,582
|
$
|
619,427
|
||||||||||
|
Consolidation of noncontrolling interest
|
—
|
—
|
—
|
—
|
—
|
—
|
—
|
3,104
|
3,104
|
|||||||||||||||||
|
Comprehensive Earnings:
|
||||||||||||||||||||||||||
|
Net earnings
|
—
|
—
|
—
|
—
|
94,836
|
—
|
—
|
3,435
|
98,271
|
|||||||||||||||||
|
Change in unrealized investment gains, net of $(511) tax
|
—
|
—
|
—
|
(924
|
)
|
—
|
—
|
—
|
—
|
(924
|
)
|
|||||||||||||||
|
Total comprehensive earnings
|
97,347
|
|||||||||||||||||||||||||
|
Common stock issued for stock offering
|
5,750,000
|
6
|
104,528
|
—
|
—
|
—
|
—
|
—
|
104,534
|
|||||||||||||||||
|
Common stock issued for employee benefit plans
|
828,654
|
—
|
4,254
|
—
|
—
|
—
|
—
|
—
|
4,254
|
|||||||||||||||||
|
Issuance of stock warrants
|
—
|
—
|
296
|
—
|
—
|
—
|
—
|
—
|
296
|
|||||||||||||||||
|
Common stock repurchases
|
—
|
—
|
—
|
—
|
—
|
141,203
|
(3,224)
|
—
|
(3,224
|
)
|
||||||||||||||||
|
Stock compensation expense
|
—
|
—
|
13,874
|
—
|
—
|
—
|
—
|
—
|
13,874
|
|||||||||||||||||
|
Excess tax benefits from stock compensation
|
—
|
—
|
868
|
—
|
—
|
—
|
—
|
—
|
868
|
|||||||||||||||||
|
Redemption / purchase of noncontrolling interest
|
—
|
—
|
(21,420)
|
—
|
—
|
—
|
—
|
(14,056)
|
(35,476
|
)
|
||||||||||||||||
|
Distributions to noncontrolling interest
|
—
|
—
|
—
|
—
|
—
|
—
|
—
|
(7,949)
|
(7,949
|
)
|
||||||||||||||||
|
Balance,
December 31, 2010
|
52,172,037
|
$
|
52
|
$
|
384,206
|
$
|
6,424
|
$
|
453,743
|
2,555,213
|
$
|
(50,486)
|
$
|
3,116
|
$
|
797,055
|
||||||||||
|
1
|
Conversion fee represents additional purchase price to noncontrolling holders of Access Health Solutions LLC for the transfer of membership to the Company’s wholly-owned subsidiary, Sunshine State Health Plan, Inc.
|
|
Year Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Cash flows from operating activities:
|
||||||||||||
|
Net earnings
|
$
|
98,271
|
$
|
86,245
|
$
|
83,497
|
||||||
|
Adjustments to reconcile net earnings to net cash provided by operating activities:
|
||||||||||||
|
Depreciation and amortization
|
52,000
|
44,004
|
35,414
|
|||||||||
|
Stock compensation expense
|
13,874
|
14,634
|
15,328
|
|||||||||
|
(Gain) loss on sale of investments, net
|
(6,337
|
)
|
(141
|
)
|
4,988
|
|||||||
|
(Gain) on sale of UHP
|
(8,201
|
)
|
—
|
—
|
||||||||
|
Impairment loss
|
5,531
|
—
|
2,546
|
|||||||||
|
Deferred income taxes
|
10,317
|
3,696
|
1,286
|
|||||||||
|
Changes in assets and liabilities:
|
||||||||||||
|
Premium and related receivables
|
(23,359
|
)
|
2,379
|
(1,548
|
)
|
|||||||
|
Other current assets
|
(3,240
|
)
|
(1,263
|
)
|
(4,244
|
)
|
||||||
|
Other assets
|
(2,028
|
)
|
9
|
(2,700
|
)
|
|||||||
|
Medical claims liability
|
(30,421
|
)
|
79,000
|
47,283
|
||||||||
|
Unearned revenue
|
25,700
|
78,345
|
(36,447
|
)
|
||||||||
|
Accounts payable and accrued expenses
|
37,398
|
(60,915
|
)
|
74,166
|
||||||||
|
Other operating activities
|
(573
|
)
|
2,202
|
2,409
|
||||||||
|
Net cash provided by operating activities
|
168,932
|
248,195
|
221,978
|
|||||||||
|
Cash flows from investing activities:
|
||||||||||||
|
Capital expenditures
|
(63,304
|
)
|
(23,721
|
)
|
(65,156
|
)
|
||||||
|
Capital expenditures of Centene Center LLC
|
(55,252
|
)
|
(59,392
|
)
|
—
|
|||||||
|
Purchase of investments
|
(615,506
|
)
|
(791,194
|
)
|
(549,652
|
)
|
||||||
|
Sales and maturities of investments
|
570,423
|
642,783
|
546,264
|
|||||||||
|
Proceeds from asset sales
|
13,420
|
—
|
—
|
|||||||||
|
Investments in acquisitions, net of cash acquired, and investment in equity method investee
|
(60,388
|
)
|
(38,563
|
)
|
(85,377
|
)
|
||||||
|
Net cash used in investing activities
|
(210,607
|
)
|
(270,087
|
)
|
(153,921
|
)
|
||||||
|
Cash flows from financing activities:
|
||||||||||||
|
Proceeds from exercise of stock options
|
3,419
|
2,365
|
5,354
|
|||||||||
|
Proceeds from borrowings
|
218,538
|
659,059
|
236,005
|
|||||||||
|
Proceeds from stock offering
|
104,534
|
—
|
—
|
|||||||||
|
Payment of long-term debt
|
(195,728
|
)
|
(616,219
|
)
|
(178,491
|
)
|
||||||
|
Purchase of noncontrolling interest
|
(48,257
|
)
|
—
|
—
|
||||||||
|
Distributions (to) from noncontrolling interest
|
(7,387
|
)
|
8,049
|
—
|
||||||||
|
Excess tax benefits from stock compensation
|
963
|
53
|
3,100
|
|||||||||
|
Common stock repurchases
|
(3,224
|
)
|
(6,304
|
)
|
(23,510
|
)
|
||||||
|
Debt issue costs
|
(769
|
)
|
(458
|
)
|
—
|
|||||||
|
Net cash provided by financing activities
|
72,089
|
46,545
|
42,458
|
|||||||||
|
Net increase in cash and cash equivalents
|
30,414
|
24,653
|
110,515
|
|||||||||
|
Cash and cash equivalents,
beginning of period
|
403,752
|
379,099
|
268,584
|
|||||||||
|
Cash and cash equivalents,
end of period
|
$
|
434,166
|
$
|
403,752
|
$
|
379,099
|
||||||
|
Supplemental disclosures of cash flow information:
|
||||||||||||
|
Interest paid
|
$
|
17,296
|
$
|
15,428
|
$
|
15,312
|
||||||
|
Income taxes paid
|
$
|
53,938
|
$
|
52,928
|
$
|
36,801
|
||||||
|
Supplemental disclosure of non-cash investing and financing activities:
|
||||||||||||
|
Contribution from noncontrolling interest
|
$
|
306
|
$
|
5,875
|
$
|
—
|
||||||
|
Capital expenditures
|
$
|
8,720
|
$
|
(1,476
|
)
|
$
|
4,175
|
|||||
|
Ÿ
|
Available for sale investments and restricted deposits: The carrying amount is stated at fair value, based on quoted market prices, where available. For securities not actively traded, fair values were estimated using values obtained from independent pricing services or quoted market prices of comparable instruments.
|
|
Ÿ
|
Senior unsecured notes: Estimated based on third-party quoted market prices for the same or similar issues.
|
|
Ÿ
|
Variable rate debt: The carrying amount of our floating rate debt approximates fair value because the interest rates adjust based on market rate adjustments.
|
|
Fixed Asset
|
Depreciation Period
|
|
|
Buildings
|
40 years
|
|
|
Computer hardware and software
|
3 – 7 years
|
|
|
Furniture and equipment
|
5 – 10 years
|
|
|
Leasehold improvements
|
1– 20 years
|
|
Intangible Asset
|
Amortization Period
|
|
|
Purchased contract rights
|
5 – 15 years
|
|
|
Provider contracts
|
5 – 10 years
|
|
|
Customer relationships
|
5 – 15 years
|
|
|
Trade names
|
7 – 20 years
|
|
|
2010
|
2009
|
2008
|
|||||||||
|
Allowances, beginning of year
|
|
$
|
1,338
|
$
|
1,304
|
$
|
467
|
|||||
|
Amounts charged to expense
|
(48
|
)
|
285
|
1,142
|
||||||||
|
Write-offs of uncollectible receivables
|
|
(1,273
|
)
|
(251
|
)
|
(305
|
)
|
|||||
|
Allowances, end of year
|
|
$
|
17
|
$
|
1,338
|
$
|
1,304
|
|||||
|
2010
|
2009
|
2008
|
||||||||||||
|
Georgia
|
17% |
Georgia
|
19% |
Georgia
|
23% | |||||||||
|
Ohio
|
13% |
Ohio
|
14% |
Ohio
|
16% | |||||||||
|
Texas
|
30% |
Texas
|
30% |
Texas
|
33% | |||||||||
In 2008, as a result of the plan to sell certain assets of UHP, the Company conducted an impairment analysis of the assets of UHP. The impairment analysis resulted in an impairment charge for fixed assets of $2,546. During the years ended December 31, 2010, 2009, and 2008 the Company incurred exit costs consisting primarily of lease termination fees and employee severance. The change in exit cost liability for UHP is summarized as follows:
|
Employee Benefits
|
Lease Termination
|
Total
|
||||||||||
|
Balance, December 31, 2008
|
$ | 444 | $ | 666 | $ | 1,110 | ||||||
|
Incurred
|
3,140 | — | 3,140 | |||||||||
|
Paid
|
(857 | ) | (400 | ) | (1,257 | ) | ||||||
|
Balance, December 31, 2009
|
2,727 | 266 | 2,993 | |||||||||
|
Incurred/(Adjustments)
|
(274 | ) | 1,010 | 736 | ||||||||
|
Paid
|
(2,186 | ) | (721 | ) | (2,907 | ) | ||||||
|
Balance, December 31, 2010
|
$ | 267 | $ | 555 | $ | 822 | ||||||
|
Year Ended December 31,
|
||||||||||||
|
|
2010
|
2009
|
2008
|
|||||||||
|
Revenues
|
|
$
|
21,757
|
$
|
145,097
|
$
|
150,638
|
|||||
|
Earnings (loss) before income taxes
|
|
$
|
8,276
|
|
$
|
(3,626
|
)
|
|
$
|
(965
|
)
|
|
|
Net earnings (loss)
|
|
$
|
3,889
|
|
$
|
(2,422
|
)
|
|
$
|
(684
|
)
|
|
|
December 31,
|
|||||||
|
2010
|
2009
|
||||||
|
Current assets
|
$ | 1,164 | $ | 7,307 | |||
|
Long term investments and restricted deposits
|
3,933 | 22,139 | |||||
|
Goodwill
|
— | 2,168 | |||||
|
Other intangible assets, net
|
— | 1,552 | |||||
|
Other assets
|
933 | 426 | |||||
|
Assets of discontinued operations
|
$ | 6,030 | $ | 33,592 | |||
|
December 31,
|
|||||||
|
2010
|
2009
|
||||||
|
Medical claims liability
|
$ | 1,464 | $ | 17,718 | |||
|
Accounts payable and accrued expenses
|
1,638 | 2,967 | |||||
|
Other liabilities
|
380 | 383 | |||||
|
Liabilities of discontinued operations
|
$ | 3,482 | $ | 21,068 | |||
|
·
|
Carolina Crescent Health Plan.
In June 2010, the Company acquired certain assets of Carolina Crescent Health Plan, a South Carolina Medicaid managed care organization for $17,993 in total consideration. The Company recorded an initial allocation of fair value that resulted in goodwill of $14,394 and other identifiable intangible assets of $3,599. The Company allocated the total consideration to assets acquired and liabilities assumed based on its initial estimates of fair value using methodologies and assumptions that it believed were reasonable. During 2010, the Company finalized the allocation of the total consideration to identifiable assets and liabilities which increased goodwill to $16,543 and decreased other identifiable intangible assets to $1,450. The acquisition is recorded in the Medicaid Managed Care segment. All of the goodwill is deductible for income tax purposes.
|
|
·
|
NovaSys Health, LLC.
In July 2010, the Company acquired certain assets and liabilities of NovaSys Health, LLC, a third party administrator in Arkansas and paid $4,330 in cash. The Company’s allocation of fair value resulted in goodwill of $1,444 and other identifiable intangible assets of $3,050 that were recorded in the Specialty Services segment. All of the goodwill is deductible for income tax purposes.
|
|
·
|
Citrus Health Care, Inc.
In December 2010, the Company acquired certain assets in non reform counties of Citrus Health Care, Inc., a Florida Medicaid and long term care health plan for $28,689. The Company performed a preliminary allocation of fair value that resulted in goodwill of $22,951 and other identifiable intangible assets of $5,738 that were recorded in the Medicaid Managed Care segment. The fair value of the acquired intangible assets is preliminary pending the final valuation of those assets.
The Company allocated the total consideration to assets acquired and liabilities assumed based on its initial estimates of fair value using methodologies and assumptions that it believed were reasonable. All of the goodwill is deductible for income tax purposes.
|
|
·
|
Access Health Solutions, LLC.
In December 2010, the Company exercised its right to obtain the remaining assets and ownership interest in Access Health Solutions, LLC, or Access, for zero dollars. Prior to the acquisition of the remaining interest, the Company had reported its investment in Access as a consolidated variable interest entity (VIE) in which the Company was the primary beneficiary. Subsequent to the acquisition of the remaining interest, Access continues to be consolidated in the Company’s Medicaid Managed Care segment results as a wholly owned subsidiary of the Company.
|
|
·
|
Centene Center LLC.
In December 2010, the Company acquired the remaining ownership interest in Centene Center LLC for $48,250. The excess purchase price over the noncontrolling interest was recorded to additional paid in capital, net of the related deferred tax asset of $12,779. Centene Center LLC is a real estate development entity created for the construction of a real estate development that includes the Company’s corporate headquarters. The Company previously reported its investment in Centene Center as a consolidated VIE. Subsequent to the acquisition of the remaining interest, Centene Center LLC continues to be consolidated as a wholly owned subsidiary of the Company. The operating results of Centene Center LLC are included in general and administrative expense of the Company’s Medicaid Managed Care segment.
|
|
·
|
Casenet, LLC.
In December 2010, the Company acquired an additional ownership interest in Casenet, LLC for total consideration of $6,619, bringing its ownership interest to 68%. Casenet, LLC is a provider of care management solutions that automate the clinical, administrative, and technical components of care management programs. The Company performed an initial allocation of total consideration to assets acquired and liabilities assumed based on its initial estimates of fair value using methodologies and assumptions that it believed were reasonable. The initial allocation resulted in goodwill of $1,752 and other identifiable intangible assets of $4,500 that were recorded in the Specialty Services segment. The fair value of the acquired intangible assets is preliminary pending the final valuation of those assets.
The goodwill is not deductible for income tax purposes.
|
|
·
|
Access.
In July 2007, the Company acquired a 49% ownership interest in Access, a Medicaid managed care entity in Florida. The Company accounted for its investment in Access using the equity method of accounting through December 31, 2008. During the quarter ended March 31, 2009, the Company began presenting its investment in Access as a consolidated subsidiary in its financial statements. The consolidation of Access resulted in goodwill of approximately $43,400, and other identified intangible assets of approximately $5,400. In 2009, the Company paid an additional $33,927 conversion fee for the transfer of membership from Access to the Company’s wholly-owned subsidiary, Sunshine State Health Plan, Inc.
|
|
·
|
Additional 2009 Acquisitions
. The Company acquired assets of the following entities: Pediatric Associates LLC, effective February 2009, Amerigroup Community Care of South Carolina, Inc., effective March 2009 and InSpeech, Inc., effective July 2009. The Company paid a total of approximately $12,500 in cash for these acquisitions. Goodwill of approximately $9,500 and other identifiable intangible assets of approximately $1,500 were included in the Medicaid Managed Care segment and other identifiable intangible assets of $1,700 were included in the Specialty Services segment, all of which is deductible for income tax purposes.
|
|
·
|
Celtic Insurance Company.
On July 1, 2008, the Company acquired Celtic Insurance Company, or
Celtic, a health insurance carrier focused on the individual health insurance market. The Company paid approximately $82,100 in cash and related transaction costs, net of unregulated cash acquired. In conjunction with the closing of the acquisition, Celtic paid to the Company an extraordinary dividend of $31,411 in July 2008. The results of operations for Celtic are included in the Specialty Services segment of the consolidated financial statements since July 1, 2008.
|
|
December 31, 2010
|
December 31, 2009
|
||||||||||||||||||||||
|
Amortized Cost
|
Gross Unrealized Gains
|
Gross Unrealized Losses
|
Fair Value
|
Amortized Cost
|
Gross Unrealized Gains
|
Gross Unrealized Losses
|
Fair Value
|
||||||||||||||||
|
U.S. Treasury securities and obligations of U.S. government corporations and agencies
|
$
|
28,665
|
|
$
|
510
|
|
$
|
(140
|
)
|
$
|
29,035
|
$
|
27,080
|
|
$
|
213
|
|
$
|
(5
|
)
|
$
|
27,288
|
|
|
Corporate securities
|
197,577
|
|
3,124
|
|
(586
|
)
|
200,115
|
153,478
|
|
581
|
|
(940
|
)
|
153,119
|
|||||||||
|
Restricted certificates of deposit
|
6,814
|
|
—
|
|
—
|
6,814
|
4,958
|
|
—
|
|
—
|
4,958
|
|||||||||||
|
Restricted cash equivalents
|
8,814
|
|
—
|
|
—
|
8,814
|
7,284
|
|
—
|
|
—
|
7,284
|
|||||||||||
|
Municipal securities:
|
|||||||||||||||||||||||
|
General obligation
|
109,866
|
|
3,601
|
|
(6
|
)
|
113,461
|
141,039
|
|
6,249
|
|
(3
|
)
|
147,285
|
|||||||||
|
Pre-refunded
|
32,442
|
|
756
|
|
—
|
33,198
|
39,928
|
|
950
|
|
(25
|
)
|
40,853
|
||||||||||
|
Revenue
|
100,198
|
|
2,781
|
|
(15
|
)
|
102,964
|
119,488
|
|
4,429
|
|
(3
|
)
|
123,914
|
|||||||||
|
Variable rate demand notes
|
106,540
|
|
—
|
|
—
|
106,540
|
33,500
|
|
—
|
|
—
|
33,500
|
|||||||||||
|
Asset backed securities
|
17,391
|
243
|
(43
|
)
|
17,591
|
19,934
|
61
|
—
|
19,995
|
||||||||||||||
|
Reserve Primary fund
|
—
|
|
—
|
|
—
|
—
|
2,444
|
—
|
|
—
|
2,444
|
||||||||||||
|
Cost method investments and equity method securities
|
7,060
|
—
|
|
—
|
7,060
|
9,751
|
312
|
|
(170
|
)
|
9,893
|
||||||||||||
|
Life insurance contracts
|
14,391
|
—
|
|
—
|
14,391
|
14,650
|
—
|
|
—
|
14,650
|
|||||||||||||
|
Total
|
$
|
629,758
|
|
$
|
11,015
|
|
$
|
(790
|
)
|
$
|
639,983
|
$
|
573,534
|
|
$
|
12,795
|
|
$
|
(1,146
|
)
|
$
|
585,183
|
|
|
December 31, 2010
|
December 31, 2009
|
||||||||||||||||||||||||||||||
|
Less Than 12 Months
|
12 Months or More
|
Less Than 12 Months
|
12 Months or More
|
||||||||||||||||||||||||||||
|
Unrealized Losses
|
Fair Value
|
Unrealized Losses
|
Fair Value
|
Unrealized Losses
|
Fair Value
|
Unrealized Losses
|
Fair Value
|
||||||||||||||||||||||||
|
U.S. Treasury securities and obligations of U.S. government corporations and agencies
|
$ | (140 | ) | $ | 9,246 | $ | — | $ | — | $ | (5 | ) | $ | 785 | $ | — | $ | — | |||||||||||||
|
Corporate securities
|
(586 | ) | 40,341 | — | — | (901 | ) | 99,418 | (39 | ) | 892 | ||||||||||||||||||||
|
Municipal securities:
|
|||||||||||||||||||||||||||||||
|
General obligation
|
(6 | ) | 1,131 | — | — | (3 | ) | 956 | — | — | |||||||||||||||||||||
|
Pre-refunded
|
— | — | — | — | (25 | ) | 7,811 | — | — | ||||||||||||||||||||||
|
Revenue
|
(15 | ) | 2,419 | — | — | (3 | ) | 916 | — | — | |||||||||||||||||||||
|
Equity securities
|
— | — | — | — | (84 | ) | 527 | (86 | ) | 629 | |||||||||||||||||||||
|
Asset backed securities
|
(43 | ) | 5,276 | — | — | — | — | — | — | ||||||||||||||||||||||
|
Total
|
$ | (790 | ) | $ | 58,413 | $ | — | $ | — | $ | (1,021 | ) | $ | 110,413 | $ | (125 | ) | $ | 1,521 | ||||||||||||
|
Investments
|
Restricted Deposits
|
|||||||||||||||
|
Amortized
Cost
|
Fair
Value
|
Amortized
Cost
|
Fair
Value
|
|||||||||||||
|
One year or less
|
$ | 21,141 | $ | 21,346 | $ | 17,387 | $ | 17,392 | ||||||||
|
One year through five years
|
464,270 | 474,255 | 5,368 | 5,366 | ||||||||||||
|
Five years through ten years
|
39,732 | 39,731 | — | — | ||||||||||||
|
Greater than ten years
|
81,860 | 81,893 | — | — | ||||||||||||
|
Total
|
$ | 607,003 | $ | 617,225 | $ | 22,755 | $ | 22,758 | ||||||||
|
Investments
|
Restricted Deposits
|
|||||||||||||||
|
Amortized
Cost
|
Fair
Value
|
Amortized
Cost
|
Fair
Value
|
|||||||||||||
|
One year or less
|
$ | 39,230 | $ | 39,554 | $ | 17,737 | $ | 17,758 | ||||||||
|
One year through five years
|
456,041 | 467,112 | 2,311 | 2,374 | ||||||||||||
|
Five years through ten years
|
28,597 | 28,780 | — | — | ||||||||||||
|
Greater than ten years
|
29,618 | 29,605 | — | — | ||||||||||||
|
Total
|
$ | 553,486 | $ | 565,051 | $ | 20,048 | $ | 20,132 | ||||||||
|
|
2010
|
2009 |
2008
|
|||||||
|
Gross realized gains
|
|
$
|
6,036
|
$ |
1,252
|
$
|
1,364
|
|||
|
Gross realized losses
|
|
(270
|
)
|
(1,111
|
)
|
(5,654
|
)
|
|||
|
Impairment of investment
|
(5,531
|
)
|
—
|
—
|
||||||
|
Net realized gains (losses)
|
|
$
|
235
|
$ |
141
|
$
|
(4,290
|
)
|
||
|
Level Input:
|
|
Input Definition:
|
|
Level I
|
|
Inputs are unadjusted, quoted prices for identical assets or liabilities in active markets at the measurement date.
|
|
Level II
|
|
Inputs other than quoted prices included in Level I that are observable for the asset or liability through corroboration with market data at the measurement date.
|
|
Level III
|
|
Unobservable inputs that reflect management’s best estimate of what market participants would use in pricing the asset or liability at the measurement date.
|
|
|
Level I
|
|
Level II
|
|
Level III
|
|
Total
|
|||||
|
Cash and cash equivalents
|
$
|
433,914
|
$
|
―
|
$
|
―
|
$
|
433,914
|
||||
|
Investments available for sale:
|
||||||||||||
|
U.S. Treasury securities and obligations of U.S. government corporations and agencies
|
|
$
|
14,809
|
|
$
|
7,096
|
|
$
|
―
|
|
$
|
21,905
|
|
Corporate securities
|
|
―
|
|
200,115
|
|
―
|
200,115
|
|||||
|
Municipal securities:
|
||||||||||||
|
General obligation
|
―
|
|
113,461
|
|
―
|
113,461
|
||||||
|
Pre-refunded
|
―
|
|
33,198
|
|
―
|
33,198
|
||||||
|
Revenue
|
―
|
|
102,964
|
|
―
|
102,964
|
||||||
|
Variable rate demand notes
|
|
―
|
|
106,540
|
|
―
|
106,540
|
|||||
|
Asset backed securities
|
―
|
17,591
|
―
|
17,591
|
||||||||
|
Total investments
|
$
|
14,809
|
|
$
|
580,965
|
|
$
|
―
|
$
|
595,774
|
||
|
Restricted deposits available for sale:
|
||||||||||||
|
Cash and cash equivalents
|
$
|
8,814
|
$
|
―
|
$
|
―
|
$
|
8,814
|
||||
|
Certificates of deposit
|
6,814
|
―
|
―
|
6,814
|
||||||||
|
U.S. Treasury securities and obligations of U.S. government corporations and agencies
|
7,130
|
―
|
―
|
7,130
|
||||||||
|
Total restricted deposits
|
$
|
22,758
|
$
|
―
|
$
|
―
|
$
|
22,758
|
||||
|
Total assets at fair value
|
$
|
471,481
|
$
|
580,965
|
$
|
―
|
$
|
1,052,446
|
||||
|
Level I
|
Level II
|
Level III
|
Total
|
|||||||||
|
Cash and cash equivalents
|
$ | 400,951 | $ | ― | $ | ― | $ | 400,951 | ||||
|
Investments available for sale:
|
||||||||||||
|
U.S. Treasury securities and obligations of U.S. government corporations and agencies
|
$ | 16,635 | $ | 2,764 | $ | ― | $ | 19,399 | ||||
|
Corporate securities
|
― | 152,919 | ― | 152,919 | ||||||||
|
Municipal securities:
|
||||||||||||
|
General obligation
|
― | 147,285 | ― | 147,285 | ||||||||
|
Pre-refunded
|
― | 40,853 | ― | 40,853 | ||||||||
|
Revenue
|
― | 123,914 | ― | 123,914 | ||||||||
|
Variable rate demand notes
|
― | 33,500 | ― | 33,500 | ||||||||
|
Equity securities
|
3,585 | ― | ― | 3,585 | ||||||||
|
Asset backed securities
|
― | 19,995 | ― | 19,995 | ||||||||
|
Total investments
|
$ | 20,220 | $ | 521,230 | $ | ― | $ | 541,450 | ||||
|
Restricted deposits available for sale:
|
||||||||||||
|
Cash and cash equivalents
|
$ | 7,285 | $ | ― | $ | ― | $ | 7,285 | ||||
|
Certificates of deposit
|
4,958 | ― | ― | 4,958 | ||||||||
|
U.S. Treasury securities and obligations of U.S. government corporations and agencies
|
7,889 | ― | ― | 7,889 | ||||||||
|
Total restricted deposits
|
$ | 20,132 | $ | ― | $ | ― | $ | 20,132 | ||||
|
Total assets at fair value
|
$ | 441,303 | $ | 521,230 | $ | ― | $ | 962,533 | ||||
|
|
2010
|
2009
|
|||||
|
Computer software
|
|
$
|
141,918
|
$
|
113,416
|
||
|
Building
|
|
171,072
|
|
104,786
|
|||
|
Land
|
|
44,282
|
40,639
|
||||
|
Computer hardware
|
35,639
|
31,651
|
|||||
|
Furniture and office equipment
|
|
33,812
|
24,012
|
||||
|
Leasehold improvements
|
|
38,247
|
19,800
|
||||
|
|
464,970
|
334,304
|
|||||
|
Less accumulated depreciation
|
|
(138,629)
|
|
(103,883)
|
|||
|
Property, software and equipment, net
|
|
$
|
326,341
|
$
|
230,421
|
||
|
Medicaid Managed Care
|
Specialty
Services
|
Total
|
||||||||||
|
Balance as of December 31, 2008
|
$ | 51,548 | $ | 111,832 | $ | 163,380 | ||||||
|
Acquisitions
|
59,515 | 1,692 | 61,207 | |||||||||
|
Balance as of December 31, 2009
|
$ | 111,063 | $ | 113,524 | $ | 224,587 | ||||||
|
Acquisitions
|
45,385 | 8,079 | 53,464 | |||||||||
|
Balance as of December 31, 2010
|
$ | 156,448 | $ | 121,603 | $ | 278,051 | ||||||
|
|
Weighted
Average Life
in Years
|
||||||||||
|
|
2010
|
2009
|
2010
|
2009
|
|||||||
|
Purchased contract rights
|
|
$
|
20,185
|
$
|
12,997
|
6.9
|
7.7
|
||||
|
Provider contracts
|
|
2,578
|
1,078
|
10.0
|
9.9
|
||||||
|
Customer relationships
|
16,056
|
15,845
|
7.7
|
7.3
|
|||||||
|
Trade names
|
|
5,595
|
5,545
|
18.9
|
19.0
|
||||||
|
Intangible assets
|
|
44,414
|
35,465
|
8.9
|
9.4
|
||||||
|
Less accumulated amortization:
|
|
||||||||||
|
Purchased contract rights
|
|
(7,053
|
)
|
(5,752
|
)
|
||||||
|
Provider contracts
|
|
(697
|
)
|
(515
|
)
|
||||||
|
Customer relationships
|
(6,278
|
)
|
(5,741
|
)
|
|||||||
|
Trade names
|
|
(1,277
|
)
|
(978
|
)
|
||||||
|
Total accumulated amortization
|
|
(15,305
|
)
|
(12,986
|
)
|
||||||
|
Intangible assets, net
|
|
$
|
29,109
|
$
|
22,479
|
||||||
|
Year
|
Expense
|
|||
|
2011
|
$ | 5,200 | ||
|
2012
|
5,100 | |||
|
2013
|
4,600 | |||
|
2014
|
4,200 | |||
|
2015
|
3,400 | |||
|
|
2010
|
2009
|
2008
|
||||||
|
Current provision:
|
|
||||||||
|
Federal
|
|
$
|
46,259
|
$
|
41,310
|
$
|
53,543
|
||
|
State and local
|
|
6,868
|
5,578
|
6,726
|
|||||
|
Total current provision
|
|
53,127
|
46,888
|
60,269
|
|||||
|
Deferred provision
|
|
6,773
|
1,953
|
(7,834)
|
|||||
|
Total provision for income taxes
|
$
|
59,900
|
$
|
48,841
|
$
|
52,435
|
|||
|
|
2010
|
2009
|
2008
|
||||||||
|
Earnings from continuing operations, before income tax expense
|
|
$
|
154,282
|
$
|
137,508
|
$
|
136,616
|
||||
|
Less noncontrolling interest
|
|
3,435
|
2,574
|
—
|
|||||||
|
Earnings from continuing operations, less noncontrolling interest, before income tax expense
|
150,847
|
134,934
|
136,616
|
||||||||
|
U.S. federal statutory rate
|
35.0%
|
35.0%
|
35.0%
|
||||||||
|
Tax provision at the U.S. federal statutory rate
|
52,797
|
47,227
|
47,816
|
||||||||
|
State income taxes, net of federal income tax benefit
|
|
6,231
|
2,419
|
4,938
|
|||||||
|
Other, net
|
872
|
(805
|
)
|
(319)
|
|||||||
|
Income tax expense
|
|
$
|
59,900
|
$
|
48,841
|
$
|
52,435
|
||||
|
Effective tax rate
|
39.7%
|
36.2%
|
38.4%
|
||||||||
|
2010
|
2009
|
|||||||
|
Deferred tax assets:
|
||||||||
|
Current:
|
||||||||
|
Medical claims liability and other accruals
|
$ | 25,418 | $ | 29,487 | ||||
|
Unearned premium and other deferred revenue
|
8,934 | 6,734 | ||||||
|
Other
|
1,999 | 2,633 | ||||||
|
Current deferred tax assets
|
36,351 | 38,854 | ||||||
|
Valuation allowance
|
(741 | ) | ― | |||||
|
Net current deferred tax assets
|
$ | 35,610 | $ | 38,854 | ||||
|
Non-current deferred tax assets:
|
||||||||
|
State net operating loss carry forward
|
$ | 4,841 | $ | 4,408 | ||||
|
Purchase of noncontrolling interest
|
13,223 | ― | ||||||
|
Investment in partnerships
|
― | 6,071 | ||||||
|
Stock compensation
|
13,676 | 13,915 | ||||||
|
Other
|
8,599 | 5,553 | ||||||
|
Non-current deferred tax assets
|
40,339 | 29,947 | ||||||
|
Valuation allowance
|
(4,400 | ) | (2,140 | ) | ||||
|
Net non-current deferred tax assets
|
$ | 35,939 | $ | 27,807 | ||||
|
Deferred tax liabilities:
|
||||||||
|
Current:
|
||||||||
|
Prepaid assets and other
|
$ | 4,350 | $ | 3,705 | ||||
|
Net current deferred tax liabilities
|
$ | 4,350 | $ | 3,705 | ||||
|
Non-current deferred tax liabilities:
|
||||||||
|
Intangible assets
|
$ | 11,519 | $ | 9,837 | ||||
|
Depreciation and amortization
|
34,743 | 38,302 | ||||||
|
Unrealized gain on investments
|
3,613 | 4,114 | ||||||
|
Other
|
2,777 | 85 | ||||||
|
Net non-current deferred tax liabilities
|
$ | 52,652 | $ | 52,338 | ||||
|
Net deferred tax assets
|
$ | 14,547 | $ | 10,618 | ||||
|
Balance as of December 31, 2009
|
|
$
|
3,991
|
|
|
Increase based on tax positions during the current year
|
|
232
|
||
|
Decreases based on tax positions taken in a prior period
|
(2,556
|
)
|
||
|
Balance as of December 31, 2010
|
|
$
|
1,667
|
|
Year Ended December 31,
|
|||||||||
|
|
2010
|
2009
|
2008
|
||||||
|
Balance, January 1,
|
|
$
|
470,932
|
$
|
384,360
|
$
|
323,741
|
||
|
Acquisitions
|
|
—
|
—
|
15,398
|
|||||
|
Incurred related to:
|
|||||||||
|
Current year
|
|
3,582,463
|
3,216,533
|
2,659,036
|
|||||
|
Prior years
|
|
(68,069
|
)
|
(53,010
|
)
|
(18,701)
|
|||
|
Total incurred
|
|
3,514,394
|
3,163,523
|
2,640,335
|
|||||
|
Paid related to:
|
|||||||||
|
Current year
|
|
3,133,527
|
2,752,983
|
2,292,150
|
|||||
|
Prior years
|
|
395,034
|
323,968
|
302,964
|
|||||
|
Total paid
|
|
3,528,561
|
3,076,951
|
2,595,114
|
|||||
|
Balance, December 31,
|
|
$
|
456,765
|
$
|
470,932
|
$
|
384,360
|
||
|
2010
|
2009
|
|||||||
|
Senior notes
|
$ | 175,000 | $ | 175,000 | ||||
|
Revolving credit agreement
|
60,000 | 84,000 | ||||||
|
Mortgage notes payable
|
89,500 | 9,900 | ||||||
|
Capital leases
|
6,141 | 6,272 | ||||||
|
Joint venture construction loan
|
― | 32,559 | ||||||
|
Total debt
|
330,641 | 307,731 | ||||||
|
Less current portion
|
(2,817 | ) | (646 | ) | ||||
|
Long-term debt
|
$ | 327,824 | $ | 307,085 | ||||
|
2011
|
$ | 2,817 | ||
|
2012
|
3,227 | |||
|
2013
|
3,269 | |||
|
2014
|
186,318 | |||
|
2015
|
3,174 | |||
|
Thereafter
|
131,836 | |||
|
Total
|
$ | 330,641 |
|
Shares
|
Weighted
Average
Exercise
Price
|
Aggregate Intrinsic Value
|
Weighted
Average Remaining
Contractual
Term
|
||||||||
|
Outstanding as of December 31, 2009
|
3,460,755
|
$
|
20.31
|
||||||||
|
Granted
|
10,000
|
24.12
|
|||||||||
|
Exercised
|
(202,734)
|
12.99
|
|||||||||
|
Forfeited
|
(129,500)
|
22.38
|
|||||||||
|
Outstanding as of December 31, 2010
|
3,138,521
|
$
|
20.71
|
$
|
15,395
|
4.7
|
|||||
|
Exercisable as of December 31, 2010
|
2,743,754
|
$
|
20.55
|
$
|
13,987
|
4.3
|
|||||
|
Year Ended December 31,
|
|||||||||
|
2010
|
2009
|
2008
|
|||||||
|
Expected life (in years)
|
5.8 | 5.8 | 5.8 | ||||||
|
Risk-free interest rate
|
2.7% | 2.2% | 3.0% | ||||||
|
Expected volatility
|
48.2% | 50.9% | 50.3% | ||||||
|
Expected dividend yield
|
0% | 0% | 0% | ||||||
|
Year Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Weighted-average fair value of options granted
|
$ | 11.60 | $ | 8.76 | $ | 9.27 | ||||||
|
Total intrinsic value of stock options exercised
|
$ | 1,999 | $ | 2,192 | $ | 3,529 | ||||||
|
Shares
|
Weighted
Average
Grant Date
Fair Value
|
|||||||
|
Non-vested balance as of December 31, 2009
|
1,691,061
|
$
|
20.73
|
|||||
|
Granted
|
839,635
|
23.86
|
||||||
|
Vested
|
(644,261
|
)
|
20.48
|
|||||
|
Forfeited
|
(18,400
|
)
|
19.20
|
|||||
|
Non-vested balance as of December 31, 2010
|
1,868,035
|
$
|
22.62
|
|||||
|
2011
|
$ | 18,444 | ||
|
2012
|
14,874 | |||
|
2013
|
10,245 | |||
|
2014
|
8,085 | |||
|
2015
|
6,285 | |||
|
Thereafter
|
9,864 | |||
| $ | 67,797 |
|
2010
|
2009
|
2008
|
||||||||||
|
Earnings (loss) attributable to Centene Corporation common shareholders:
|
||||||||||||
|
Earnings from continuing operations, net of tax
|
$ | 90,947 | $ | 86,093 | $ | 84,181 | ||||||
|
Discontinued operations, net of tax
|
3,889 | (2,422 | ) | (684 | ) | |||||||
|
Net earnings
|
$ | 94,836 | $ | 83,671 | $ | 83,497 | ||||||
|
Shares used in computing per share amounts:
|
||||||||||||
|
Weighted average number of common shares outstanding
|
48,754,947 | 43,034,791 | 43,275,187 | |||||||||
|
Common stock equivalents (as determined by applying the treasury stock method)
|
1,692,941 | 1,281,676 | 1,123,768 | |||||||||
|
Weighted average number of common shares and potential dilutive common shares outstanding
|
50,447,888 | 44,316,467 | 44,398,955 | |||||||||
|
Net earnings (loss) per share attributable to Centene Corporation:
|
||||||||||||
|
Basic:
|
||||||||||||
|
Continuing operations
|
$ | 1.87 | $ | 2.00 | $ | 1.95 | ||||||
|
Discontinued operations
|
0.08 | (0.06 | ) | (0.02 | ) | |||||||
|
Earnings per common share
|
$ | 1.95 | $ | 1.94 | $ | 1.93 | ||||||
|
Diluted:
|
||||||||||||
|
Continuing operations
|
$ | 1.80 | $ | 1.94 | $ | 1.90 | ||||||
|
Discontinued operations
|
0.08 | (0.05 | ) | (0.02 | ) | |||||||
|
Earnings per common share
|
$ | 1.88 | $ | 1.89 | $ | 1.88 | ||||||
|
Medicaid
Managed Care
|
Specialty
Services
|
Eliminations
|
Consolidated
Total
|
|||||||||||||
|
Premium and service revenues from external customers
|
$ | 3,679,807 | $ | 604,026 | $ | — | $ | 4,283,833 | ||||||||
|
Premium and service revenues from internal customers
|
60,676 | 508,157 | (568,833 | ) | — | |||||||||||
|
Total premium and service revenues
|
3,740,483 | 1,112,183 | (568,833 | ) | 4,283,833 | |||||||||||
|
Earnings from operations
|
117,106 | 39,963 | — | 157,069 | ||||||||||||
|
Total assets
|
1,552,886 | 390,996 | — | 1,943,882 | ||||||||||||
|
Stock compensation expense
|
12,716 | 1,158 | — | 13,874 | ||||||||||||
|
Depreciation expense
|
33,502 | 3,629 | — | 37,131 | ||||||||||||
|
Total capital expenditures
|
116,208 | 2,348 | — | 118,556 | ||||||||||||
|
Medicaid
Managed Care
|
Specialty
Services
|
Eliminations
|
Consolidated
Total
|
|||||||||||||
|
Premium and service revenues from external customers
|
$ | 3,398,009 | $ | 480,274 | $ | — | $ | 3,878,283 | ||||||||
|
Premium and service revenues from internal customers
|
66,763 | 569,191 | (635,954 | ) | — | |||||||||||
|
Total premium and service revenues
|
3,464,772 | 1,049,465 | (635,954 | ) | 3,878,283 | |||||||||||
|
Earnings from operations
|
99,307 | 38,828 | — | 138,135 | ||||||||||||
|
Total assets
|
1,330,987 | 371,377 | — | 1,702,364 | ||||||||||||
|
Stock compensation expense
|
13,285 | 1,349 | — | 14,634 | ||||||||||||
|
Depreciation expense
|
29,007 | 4,096 | — | 33,103 | ||||||||||||
|
Total capital expenditures
|
80,867 | 2,246 | — | 83,113 | ||||||||||||
|
Medicaid
Managed Care
|
Specialty
Services
|
Eliminations
|
Consolidated
Total
|
|||||||||||||
|
Premium and service revenues from external customers
|
$ | 2,931,894 | $ | 342,419 | $ | — | $ | 3,274,313 | ||||||||
|
Premium and service revenues from internal customers
|
60,451 | 474,061 | (534,512 | ) | — | |||||||||||
|
Total premium and service revenues
|
2,992,345 | 816,480 | (534,512 | ) | 3,274,313 | |||||||||||
|
Earnings from operations
|
108,363 | 23,198 | — | 131,561 | ||||||||||||
|
Total assets
|
1,105,610 | 345,542 | — | 1,451,152 | ||||||||||||
|
Stock compensation expense
|
13,840 | 1,346 | — | 15,186 | ||||||||||||
|
Depreciation expense
|
25,271 | 3,182 | — | 28,453 | ||||||||||||
|
Total capital expenditures
|
58,856 | 4,635 | — | 63,491 | ||||||||||||
|
Year Ended December 31,
|
||||||||
|
2010
|
2009
|
2008
|
||||||
|
Net earnings
|
$
|
94,836
|
$
|
83,671
|
$
|
83,497
|
||
|
Reclassification adjustment, net of tax
|
(1,660)
|
252
|
252
|
|||||
|
Change in unrealized gains on investments available for sale, net of tax
|
736
|
3,944
|
1,329
|
|||||
|
Total change
|
(924)
|
4,196
|
1,581
|
|||||
|
Comprehensive earnings
|
93,912
|
87,867
|
85,078
|
|||||
|
Comprehensive earnings attributable to the noncontrolling interest
|
3,435
|
2,574
|
—
|
|||||
|
Comprehensive earnings attributable to Centene Corporation
|
$
|
90,477
|
$
|
85,293
|
$
|
85,078
|
||
|
For the Quarter Ended
|
||||||||||||||||
|
March 31,
2010
|
June 30,
2010
|
September 30,
2010
|
December 31,
2010
|
|||||||||||||
|
Total revenues
|
$ | 1,068,721 | $ | 1,076,772 | $ | 1,121,861 | $ | 1,180,969 | ||||||||
|
Amounts attributable to Centene Corporation common shareholders:
|
||||||||||||||||
|
Earnings from continuing operations, net of income tax expense
|
20,082 | 22,999 | 22,402 | 25,464 | ||||||||||||
|
Discontinued operations, net of income tax expense (benefit)
|
3,920 | (226 | ) | 260 | (65 | ) | ||||||||||
|
Net earnings
|
$ | 24,002 | $ | 22,773 | $ | 22,662 | $ | 25,399 | ||||||||
|
Net earnings per share attributable to Centene Corporation:
|
||||||||||||||||
|
Basic:
|
||||||||||||||||
|
Continued operations
|
$ | 0.43 | $ | 0.46 | $ | 0.46 | $ | 0.52 | ||||||||
|
Discontinued operations
|
0.08 | — | — | — | ||||||||||||
|
Basic earnings per common share
|
$ | 0.51 | $ | 0.46 | $ | 0.46 | $ | 0.52 | ||||||||
|
Diluted:
|
||||||||||||||||
|
Continued operations
|
$ | 0.41 | $ | 0.45 | $ | 0.44 | $ | 0.50 | ||||||||
|
Discontinued operations
|
0.08 | — | — | — | ||||||||||||
|
Diluted earnings per common share
|
$ | 0.49 | $ | 0.45 | $ | 0.44 | $ | 0.50 | ||||||||
|
Period end at-risk membership
|
1,471,300 | 1,534,600 | 1,473,800 | 1,533,500 | ||||||||||||
|
For the Quarter Ended
|
||||||||||||||||
|
March 31,
2009
|
June 30,
2009
|
September 30,
2009
|
December 31,
2009
|
|||||||||||||
|
Total revenues
|
$ | 932,435 | $ | 1,039,469 | $ | 1,038,234 | $ | 1,092,726 | ||||||||
|
Amounts attributable to Centene Corporation common shareholders:
|
||||||||||||||||
|
Earnings from continuing operations, net of income tax expense
|
18,907 | 20,715 | 22,728 | 23,743 | ||||||||||||
|
Discontinued operations, net of income tax (benefit) expense
|
(449 | ) | (485 | ) | (1,460 | ) | (28 | ) | ||||||||
|
Net earnings
|
$ | 18,458 | $ | 20,230 | $ | 21,268 | $ | 23,715 | ||||||||
|
Net earnings (loss) per share attributable to Centene Corporation:
|
||||||||||||||||
|
Basic:
|
||||||||||||||||
|
Continued operations
|
$ | 0.44 | $ | 0.48 | $ | 0.53 | $ | 0.55 | ||||||||
|
Discontinued operations
|
(0.01 | ) | (0.01 | ) | (0.04 | ) | — | |||||||||
|
Basic earnings per common share
|
$ | 0.43 | $ | 0.47 | $ | 0.49 | $ | 0.55 | ||||||||
|
Diluted:
|
||||||||||||||||
|
Continued operations
|
$ | 0.43 | $ | 0.47 | $ | 0.51 | $ | 0.53 | ||||||||
|
Discontinued operations
|
(0.01 | ) | (0.01 | ) | (0.03 | ) | — | |||||||||
|
Diluted earnings per common share
|
$ | 0.42 | $ | 0.46 | $ | 0.48 | $ | 0.53 | ||||||||
|
Period end at-risk membership
|
1,249,600 | 1,291,400 | 1,388,900 | 1,458,200 | ||||||||||||
|
December 31,
|
||||||||
|
2010
|
2009
|
|||||||
|
ASSETS
|
||||||||
|
Current assets:
|
||||||||
|
Cash and cash equivalents
|
$ | 9,380 | $ | 8,664 | ||||
|
Short-term investments, at fair value (amortized cost $560 and $1,305, respectively)
|
568 | 1,307 | ||||||
|
Other current assets
|
102,754 | 84,588 | ||||||
|
Total current assets
|
112,702 | 94,559 | ||||||
|
Long-term investments, at fair value (amortized cost $10,848 and 16,646, respectively)
|
11,109 | 17,160 | ||||||
|
Investment in subsidiaries
|
898,601 | 756,892 | ||||||
|
Other long-term assets
|
17,134 | 14,673 | ||||||
|
Total assets
|
$ | 1,039,546 | $ | 883,284 | ||||
|
LIABILITIES AND STOCKHOLDERS’ EQUITY
|
||||||||
|
Current liabilities
|
$ | 6,193 | $ | 3,785 | ||||
|
Long-term debt
|
235,000 | 259,000 | ||||||
|
Other long-term liabilities
|
1,298 | 1,072 | ||||||
|
Total liabilities
|
242,491 | 263,857 | ||||||
|
Stockholders’ equity:
|
||||||||
|
Common stock, $.001 par value; authorized 100,000,000 shares; 52,172,037 issued and 49,616,824 outstanding at December 31, 2010, and 45,593,383 issued and 43,179,373 outstanding at December 31, 2009
|
52 | 46 | ||||||
|
Additional paid-in capital
|
384,206 | 281,806 | ||||||
|
Accumulated other comprehensive income:
|
||||||||
|
Unrealized gain on investments, net of tax
|
6,424 | 7,348 | ||||||
|
Retained earnings
|
453,743 | 358,907 | ||||||
|
Treasury stock, at cost (2,555,213 and 2,414,010 shares, respectively)
|
(50,486 | ) | (47,262 | ) | ||||
|
Total Centene stockholders’ equity
|
793,939 | 600,845 | ||||||
|
Noncontrolling interest
|
3,116 | 18,582 | ||||||
|
Total stockholders’ equity
|
797,055 | 619,427 | ||||||
|
Total liabilities and stockholders’ equity
|
$ | 1,039,546 | $ | 883,284 | ||||
|
Year Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Expenses:
|
||||||||||||
|
General and administrative expenses
|
$
|
(3,502
|
)
|
$
|
(2,906
|
)
|
$
|
(6,153
|
)
|
|||
|
Other income (expense):
|
||||||||||||
|
Investment and other income
|
(4,700
|
)
|
6
|
(324
|
)
|
|||||||
|
Interest expense
|
(14,844
|
)
|
(15,692
|
)
|
(15,395
|
)
|
||||||
|
Loss before income taxes
|
(23,046
|
)
|
(18,592
|
)
|
(21,872
|
)
|
||||||
|
Income tax benefit
|
(8,576
|
)
|
(6,004
|
)
|
(7,988
|
)
|
||||||
|
Net earnings (loss) before equity in subsidiaries
|
(14,470
|
)
|
(12,588
|
)
|
(13,884
|
)
|
||||||
|
Equity in earnings from subsidiaries
|
109,306
|
96,259
|
97,381
|
|||||||||
|
Net earnings
|
$
|
94,836
|
$
|
83,671
|
$
|
83,497
|
||||||
|
Net earnings per share:
|
||||||||||||
|
Basic earnings per common share
|
$
|
1.95
|
$
|
1.94
|
$
|
1.93
|
||||||
|
Diluted earnings per common share
|
$
|
1.88
|
$
|
1.89
|
$
|
1.88
|
||||||
|
Weighted average number of shares outstanding:
|
||||||||||||
|
Basic
|
48,754,947
|
43,034,791
|
43,275,187
|
|||||||||
|
Diluted
|
50,447,888
|
44,316,467
|
44,398,955
|
|||||||||
|
Year Ended December 31,
|
||||||||||||
|
2010
|
2009
|
2008
|
||||||||||
|
Cash flows from operating activities:
|
||||||||||||
|
Cash provided by operating activities
|
$
|
23,504
|
$
|
92,711
|
$
|
37,487
|
||||||
|
Cash flows from investing activities:
|
||||||||||||
|
Net dividends from and capital contributions to subsidiaries
|
(17,172
|
)
|
(67,328
|
)
|
10,146
|
|||||||
|
Purchase of investments
|
(86,549
|
)
|
(17,181
|
)
|
(39,261
|
)
|
||||||
|
Sales and maturities of investments
|
90,121
|
9,189
|
30,779
|
|||||||||
|
Acquisitions, net of cash acquired
|
(48,656
|
)
|
(38,563
|
)
|
(91,345
|
)
|
||||||
|
Proceeds from asset sales
|
13,420
|
—
|
—
|
|||||||||
|
Net cash used in investing activities
|
(48,836
|
)
|
(113,883
|
)
|
(89,681
|
)
|
||||||
|
Cash flows from financing activities:
|
||||||||||||
|
Proceeds from borrowings
|
91,000
|
616,500
|
224,000
|
|||||||||
|
Payment of long-term debt and notes payable
|
(115,000
|
)
|
(595,500
|
)
|
(166,000
|
)
|
||||||
|
Proceeds from exercise of stock options
|
3,419
|
2,365
|
5,354
|
|||||||||
|
Common stock offering
|
104,534
|
—
|
—
|
|||||||||
|
Common stock repurchases
|
(3,224
|
)
|
(6,304
|
)
|
(23,510
|
)
|
||||||
|
Debt issue costs
|
—
|
(368
|
)
|
—
|
||||||||
|
Distribution to noncontrolling interest
|
(8,158
|
)
|
(3,170
|
)
|
—
|
|||||||
|
Contributions from noncontrolling interest
|
771
|
11,219
|
—
|
|||||||||
|
Purchase of noncontrolling interest
|
(48,257
|
)
|
—
|
—
|
||||||||
|
Excess tax benefits from stock compensation
|
963
|
53
|
3,100
|
|||||||||
|
Net cash provided by financing activities
|
26,048
|
24,795
|
42,944
|
|||||||||
|
Net increase (decrease) in cash and cash equivalents
|
716
|
3,623
|
(9,250
|
)
|
||||||||
|
Cash and cash equivalents,
beginning of period
|
8,664
|
5,041
|
14,291
|
|||||||||
|
Cash and cash equivalents,
end of period
|
$
|
9,380
|
$
|
8,664
|
$
|
5,041
|
||||||
|
(a)
|
Financial Statements and Schedules
|
|
Report of Independent Registered Public Accounting Firm
|
|
Consolidated Balance Sheets as of December 31, 2010 and 2009
|
|
Consolidated Statements of Operations for the Years Ended December 31, 2010, 2009 and 2008
|
|
Consolidated Statements of Stockholders’ Equity for the Years Ended December 31, 2010, 2009 and 2008
|
|
Consolidated Statements of Cash Flows for the Years Ended December 31, 2010, 2009 and 2008
|
|
Notes to Consolidated Financial Statements
|
|
|
INCORPORATED BY REFERENCE
1
|
|||||||||
|
EXHIBIT
NUMBER
|
|
DESCRIPTION
|
FILED WITH
THIS
FORM 10-K
|
FORM
|
FILING DATE
WITH SEC
|
EXHIBIT
NUMBER
|
||||
|
3.1
|
|
Certificate of Incorporation of Centene Corporation
|
S-1
|
October 9, 2001
|
3.2
|
|||||
|
3.1a
|
|
Certificate of Amendment to Certificate of Incorporation of Centene Corporation, dated November 8, 2001
|
S-1/A
|
November 13, 2001
|
3.2a
|
|||||
|
3.1b
|
|
Certificate of Amendment to Certificate of Incorporation of Centene Corporation as filed with the Secretary of State of the State of Delaware
|
10-Q
|
July 26, 2004
|
3.1b
|
|||||
|
3.2
|
|
By-laws of Centene Corporation
|
S-1
|
October 9, 2001
|
3.4
|
|||||
|
4.1
|
|
Rights Agreement between Centene Corporation and Mellon Investor Services LLC, as Rights Agent, dated August 30, 2002
|
8-K
|
August 30, 2002
|
4.1
|
|||||
|
4.1a
|
|
Amendment No. 1 to Rights Agreement by and between Centene Corporation and Mellon Investor Services LLC, as Rights Agent, dated April 23, 2007
|
8-K
|
April 26, 2007
|
4.1
|
|||||
|
4.2
|
|
Indenture for the 7 ¼% Senior Notes due 2014 dated March 22, 2007 among Centene Corporation and The Bank of New York Trust Company, N.A., as trustee
|
S-4
|
May 11, 2007
|
4.3
|
|||||
|
10.1
|
Contract Between the Georgia Department of Community Health and Peach State Contract for provision of Services to Georgia Healthy Families
|
8-K
|
July 22, 2005
|
10.1
|
||||||
|
10.1a
|
Amendment #1 to the Contract No. 0653 Between Georgia Department of Community Health and Peach State
|
10-Q
|
October 25, 2005
|
10.9
|
||||||
|
10.1b
|
Amendment #2 to the Contract No. 0653 Between Georgia Department of Community Health and Peach State
|
10-K
|
February 23, 2008
|
10.1b
|
||||||
|
10.1c
|
Amendment #3 to the Contract No. 0653 Between Georgia Department of Community Health and Peach State
|
10-K
|
February 23, 2009
|
10.1c
|
||||||
|
10.1d
|
Amendment #4 to the Contract No. 0653 Between Georgia Department of Community Health and Peach State
|
10-K
|
February 23, 2009
|
10.1d
|
||||||
|
10.1e
|
Amendment #6 to the Contract No. 0653 Between Georgia Department of Community Health and Peach State
|
10-K
|
February 22, 2010
|
10.1e
|
||||||
|
10.1f
|
|
Amendment #7 to the Contract No. 0653 Between Georgia Department of Community Health and Peach State
|
X
|
|||||||
|
10.1g
|
**
|
Amendment #8 to the Contract No. 0653 Between Georgia Department of Community Health and Peach State
|
X
|
|
||||||
|
10.1h
|
Notice of Extension of Contract No. 0653 between Peach State Health Plan, Inc. and Georgia Department of Community Health |
X
|
||||||||
|
10.2
|
Contract between the Texas Health and Human Services Commission and Superior HealthPlan, Inc.
|
10-K
|
February 24, 2006
|
10.5
|
||||||
|
10.2a
|
**
|
Amendment Q (Version 1.17) to Contract between the Texas Health and Human Services Commission and Superior HealthPlan, Inc.
|
X
|
|||||||
|
10.3
|
*
|
1996 Stock Plan of Centene Corporation, shares which are registered on Form S-8 – File Number 333-83190
|
S-1
|
October 9, 2001
|
10.9
|
|||||
|
10.4
|
*
|
1998 Stock Plan of Centene Corporation, shares which are registered on Form S-8 – File number 333-83190
|
S-1
|
October 9, 2001
|
10.10
|
|||||
|
10.5
|
*
|
1999 Stock Plan of Centene Corporation, shares which are registered on Form S-8 – File Number 333-83190
|
S-1
|
October 9, 2001
|
10.11
|
|||||
|
10.6
|
*
|
2000 Stock Plan of Centene Corporation, shares which are registered on Form S-8 – File Number 333-83190
|
S-1
|
October 9, 2001
|
10.12
|
|||||
|
10.7
|
*
|
2002 Employee Stock Purchase Plan of Centene Corporation, shares which are registered on Form S-8 – File Number 333-90976
|
10-Q
|
April 29, 2002
|
10.5
|
|||||
|
10.7a
|
*
|
First Amendment to the 2002 Employee Stock Purchase Plan
|
10-K
|
February 24, 2005
|
10.9a
|
|||||
|
10.7b
|
*
|
Second Amendment to the 2002 Employee Stock Purchase Plan
|
10-K
|
February 24, 2006
|
10.10b
|
|||||
|
10.8
|
*
|
Centene Corporation Amended and Restated 2003 Stock Incentive Plan, shares which are registered on Form S-8 – File Number 333-108467
|
8-K
|
April 30, 2010
|
10.1
|
|||||
|
10.9
|
*
|
Centene Corporation Non-Employee Directors Deferred Stock Compensation Plan
|
10-Q
|
October 25, 2004
|
10.1
|
|||||
|
10.9a
|
*
|
First Amendment to the Non-Employee Directors Deferred Stock Compensation Plan
|
10-K
|
February 24, 2006
|
10.12a
|
|||||
|
10.10
|
*
|
Centene Corporation Employee Deferred Compensation Plan
|
10-K
|
February 22, 1010
|
10.10
|
|||||
|
10.11
|
*
|
Centene Corporation 2007 Long-Term Incentive Plan
|
8-K
|
April 26, 2007
|
10.2
|
|||||
|
10.12
|
*
|
Centene Corporation Short-Term Executive Compensation Plan
|
X
|
|||||||
|
10.13
|
*
|
Executive Employment Agreement between Centene Corporation and Michael F. Neidorff, dated November 8, 2004
|
8-K
|
November 9, 2004
|
10.1
|
|||||
|
10.13a
|
*
|
Amendment No. 1 to Executive Employment Agreement between Centene Corporation and Michael F. Neidorff
|
10-Q
|
October 28, 2008
|
10.2
|
|||||
|
10.13b
|
*
|
Amendment No. 2 to Executive Employment Agreement between Centene Corporation and Michael F. Neidorff
|
10-Q
|
April 28, 2009
|
10.2
|
|||||
|
10.14
|
*
|
Form of Executive Severance and Change in Control Agreement
|
10-Q
|
October 28, 2008
|
10.3
|
|||||
|
10.15
|
*
|
Form of Restricted Stock Unit Agreement
|
10-Q
|
October 28, 2008
|
10.4
|
|||||
|
10.16
|
*
|
Form of Non-statutory Stock Option Agreement (Non-Employees)
|
8-K
|
July 28, 2005
|
10.3
|
|||||
|
10.17
|
*
|
Form of Non-statutory Stock Option Agreement (Employees)
|
10-Q
|
October 28, 2008
|
10.5
|
|||||
|
10.18
|
*
|
Form of Non-statutory Stock Option Agreement (Directors)
|
10-K
|
February 23, 2009
|
10.18
|
|||||
|
10.19
|
*
|
Form of Incentive Stock Option Agreement
|
10-Q
|
October 28, 2008
|
10.6
|
|||||
|
10.20
|
*
|
Form of Stock Appreciation Right Agreement
|
8-K
|
July 28, 2005
|
10.6
|
|||||
|
10.21
|
*
|
Form of Restricted Stock Agreement
|
10-Q
|
October 25, 2005
|
10.8
|
|||||
|
10.22
|
*
|
Form of Performance Based Restricted Stock Unit Agreement #1
|
10-Q
|
October 28, 2008
|
10.7
|
|||||
|
10.23
|
*
|
Form of Performance Based Restricted Stock Unit Agreement #2
|
10-K
|
February 23, 2009
|
10.23
|
|||||
|
10.24
|
*
|
Form of Long Term Incentive Plan Agreement
|
8-K
|
February 7, 2008
|
10.1
|
|||||
|
10.25
|
Credit Agreement dated as of September 14, 2004 among Centene Corporation, the various financial institutions party hereto and LaSalle Bank National Association
|
10-Q
|
October 25, 2004
|
10.2
|
||||||
|
10.25a
|
Amendment No. 2 to Credit Agreement dated as of September 14, 2004 among Centene Corporation, the various financial institutions party hereto and LaSalle Bank National Association
|
10-Q
|
October 25, 2005
|
10.11
|
||||||
|
10.25b
|
Amendment No. 3 to Credit Agreement dated as of September 14, 2004 among Centene Corporation, the various financial institutions party hereto and LaSalle Bank National Association
|
10-K
|
February 24, 2006
|
10.22b
|
||||||
|
10.25c
|
Amendment No. 4 to Credit Agreement dated as of September 14, 2004 among Centene Corporation, the various financial institutions party hereto and LaSalle Bank National Association
|
10-Q
|
July 25, 2006
|
10.2
|
||||||
|
10.25d
|
Amendment No. 5 to Credit Agreement dated as of September 14, 2004 among Centene Corporation, the various financial institutions party hereto and LaSalle Bank National Association
|
10-Q
|
October 24, 2006
|
10.1
|
||||||
|
10.25e
|
Amendment No. 6 to Credit Agreement dated as of September 14, 2004 among Centene Corporation, the various financial institutions party hereto and LaSalle Bank National Association
|
10-K
|
February 23, 2008
|
10.23e
|
||||||
|
10.25f
|
Amendment No. 7 to Credit Agreement dated as of September 14, 2004 among Centene Corporation, the various financial institutions party hereto and LaSalle Bank National Association
|
10-Q
|
July 28, 2009
|
10.1
|
||||||
|
10.26
|
**
|
Credit Agreement dated as of January 31, 2011 among Centene Corporation, the various financial institutions party hereto and Barclays Bank PLC
|
X
|
|||||||
|
12.1
|
Computation of ratio of earnings to fixed charges
|
X
|
||||||||
|
21
|
List of subsidiaries
|
X
|
||||||||
|
23
|
Consent of Independent Registered Public Accounting Firm incorporated by reference in each prospectus constituting part of the Registration Statements on Form S-3 (File Number 333-164390) and on Form S-8 (File Numbers 333-108467, 333-90976 and 333-83190)
|
X
|
||||||||
|
31.1
|
Certification Pursuant to Rule 13a-14(a) and 15d-14(a) of the Exchange Act, as Adopted Pursuant to Section 302 of the Sarbanes-Oxley Act of 2002 (Chief Executive Officer)
|
X
|
||||||||
|
31.2
|
Certification Pursuant to Rule 13a-14(a) and 15d-14(a) of the Exchange Act, as Adopted Pursuant to Section 302 of the Sarbanes-Oxley Act of 2002 (Chief Financial Officer)
|
X
|
||||||||
|
32.1
|
Certification Pursuant to 18 U.S.C. Section 1350 (Chief Executive Officer)
|
X
|
||||||||
|
32.2
|
Certification Pursuant to 18 U.S.C. Section 1350 (Chief Financial Officer)
|
X
|
||||||||
|
101.1
2
|
XBRL Taxonomy Instance Document.
|
X
|
||||||||
|
101.2
2
|
XBRL Taxonomy Extension Schema Document.
|
X
|
||||||||
|
101.3
2
|
XBRL Taxonomy Extension Calculation Linkbase Document.
|
X
|
||||||||
|
101.4
2
|
XBRL Taxonomy Extension Definition Linkbase Document.
|
X
|
||||||||
|
101.5
2
|
XBRL Taxonomy Extension Label Linkbase Document.
|
X
|
||||||||
|
101.6
2
|
XBRL Taxonomy Extension Presentation Linkbase Document.
|
X
|
||||||||
|
1
SEC File No. 001-31826 (for filings prior to October 14, 2003, the Registrant’s SEC File No. was 000-33395).
2
XBRL (Extensible Business Reporting Language) information is furnished and not filed or a part of a registration statement or prospectus for purposes of sections 11 or 12 of the Securities Act of 1933, is deemed not filed for purposes of section 18 of the Securities Exchange Act of 1934, and otherwise is not subject to liability under these sections.
*
Indicates a management contract or compensatory plan or arrangement.
**
The Company has requested confidential treatment of the redacted portions of this exhibit pursuant to Rule 24b-2 under the Securities Exchange Act of 1934, as amended, and has separately filed a complete copy of this exhibit with the Securities and Exchange Commission.
|
||||||||||
|
CENTENE CORPORATION
|
||
|
By:
|
/s/ M
ICHAEL
F. N
EIDORFF
|
|
|
Michael F. Neidorff
Chairman and Chief Executive Officer
|
||
|
Signature
|
|
Title
|
|
/s/ M
ICHAEL
F. N
EIDORFF
Michael F. Neidorff
|
|
Chairman and Chief Executive Officer
(principal executive officer)
|
|
/s/ W
ILLIAM
N. S
CHEFFEL
William N. Scheffel
|
|
Executive Vice President and Chief Financial Officer (principal financial officer)
|
|
/s/ J
EFFREY
A. S
CHWANEKE
Jeffrey A. Schwaneke
|
Vice President, Corporate Controller and Chief Accounting Officer (principal accounting officer)
|
|
|
/s/ R
OBERT
K. D
ITMORE
Robert K. Ditmore
|
|
Director
|
|
/s/ F
RED
H. E
PPINGER
Fred H. Eppinger
|
|
Director
|
|
/s/ R
ICHARD
A. G
EPHARDT
Richard A. Gephardt
|
|
Director
|
|
/s/ P
AMELA
A. J
OSEPH
Pamela A. Joseph
|
|
Director
|
|
/s/ J
OHN
R. R
OBERTS
John R. Roberts
|
|
Director
|
|
/s/ D
AVID
L. S
TEWARD
David L. Steward
|
|
Director
|
|
/s/ T
OMMY
G. T
HOMPSON
Tommy G. Thompson
|
|
Director
|